Humana 2000 Annual Report Download - page 6
Download and view the complete annual report
Please find page 6 of the 2000 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
MOMENTUM
It’s an equation of shedding non-core markets and
products, while boosting the business
with focused attention on
critical mass, improved
performance and
markets and
products with
high growth
potential.
f o c u s
9
g a i n i n g . . .
Entering 2000, Humana carried the burden of a number of markets and
products that were unprofitable and that had little chance of achieving
near-term profitability. In response, our management team moved quickly
to eliminate these “non-core” elements of our business:
We notified 17 states of our intent to exit underperforming small-group
lines of business.
We sold our unprofitable North Florida Medicaid business and, in early
2001, sold unprofitable Medicaid plans in Texas and Wisconsin.
We exited 45 counties on January 1, 2001, where the federal government’s
Medicare reimbursement rate was less than the cost of providing coverage
to Medicare+Choice beneficiaries.
We sold our PCA Workers’ Compensation business, our Workers’
Compensation Third-Party Administration business and our Nevada
HMO plan.
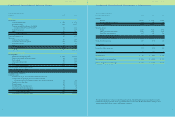
By the end of 2000, quarterly losses for the non-core markets and products
were halved from the beginning of the year, from $40 million to $20 million,
with more improvement expected in 2001.
Still, the company’s profitable core business required steady focus to
maximize its potential. The critical mass, improved performance and high
growth opportunities of core markets and products were assets that needed
to be fully exploited to revitalize our heritage as a growth company. With
this in mind:
We increased underwriting and actuarial staffs for our commercial
lines of business and improved their communication with front-line
market management.
We aligned market offices with their own dedicated teams in our service
centers, resulting in better customer service delivered by associates familiar
with the cities they serve.
We dramatically reduced our pharmacy cost trend by introducing Rx3,
a new benefit design that enhanced consumer choice while linking
consumers’ prices to their preferences.
We fostered the profitable growth of our successful ancillary businesses:
dental, TRICARE (health insurance for military retirees and dependents),
life insurance and administrative services only (ASO) plans.
We combined pricing discipline with cost management to produce
a 1.1 percent pretax margin in 2000 compared to an adjusted
0.5 percent in 1999.
Our dual commitment to pricing our products appropriately while
managing our costs effectively demonstrates the momentum gained when we
understand and respond to our customers while simultaneously focusing on
the basics of our business.
•
•
•
•
•
•
•
•
•