Humana 2000 Annual Report Download - page 8
Download and view the complete annual report
Please find page 8 of the 2000 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
In today’s society, with people increasingly taking charge of their own
health, consumers want a broad array of physicians to choose from when they
need medical care. Humana’s ChoiceCare and Classic Networks comprise
one of the largest such groups in the nation – including more than 400,000
physicians, hospitals and other providers.
But it’s no longer enough simply to provide employers and health plan
members with a list of credentialed doctors and hospitals. People are
seeking real-time, actionable information when they’re injured or sick.
When they’re well, they want fewer restrictions on their access to routine
and preventive services.
We’ve been listening to them. And we’ve acted. Our solution is access to
consumer-centric care – care that seeks to improve the health care experience
for physicians and patients, through the provision of fact-based guidance that
benefits both. In the past year, while keeping our costs in check, we’ve
reduced administrative barriers:
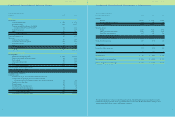
By increasing our hospital admissions automatic approval rate to
71 percent from 14 percent in 1999.
By reducing referral reviews to 10 percent from 90 percent.
By eliminating 55 percent of our prior authorization reviews on
prescription drugs.
By forging an innovative partnership with Blue Cross and Blue Shield of
Florida to create a single physician portal on the Internet to speed claims
payment and reduce paperwork. The partnership is designed to improve
efficiency for Humana and for the nearly four million Floridians who
belong to Humana and Blue Cross, along with the 30,000 Florida doctors
who care for them.
By piloting an innovative Personal Nurse feature in our Tampa, Florida
plans, whereby our most vulnerable members will be paired with a nurse
who will help them navigate options to receive the care they need, when
and where it’s needed.
The explosion of medical information available through the Internet has
presented Humana with the opportunity to partner with our members –
distilling, analyzing and explaining, in consumer-friendly terms, what the
health care system means to an individual member confronting his or her
unique health issues. It’s a challenge we’ve eagerly accepted as another way
to gain momentum in meeting customer needs.
c o n n e c t
MOMENTUM
Providing timely, actionable information
to our customers and
physicians helps us
form a strong
bond with
these key
s ta ke h o l d e r s .
13
g a i n i n g . . .
•
•
•
•
•