Health Net 2014 Annual Report Download - page 135
Download and view the complete annual report
Please find page 135 of the 2014 Health Net annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.HEALTH NET, INC.
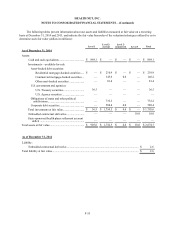
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
F-25
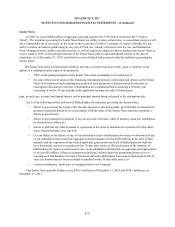
Risk Corridor—The temporary risk corridor program will be in place for three years and applies to individual
and small group business operating both inside and outside of the exchanges. The risk corridor provisions limit health
insurers' gains and losses by comparing allowable medical costs to a target amount, each defined/prescribed by HHS,
and sharing the risk for allowable costs with the federal government. Variances from the target exceeding certain
thresholds may result in HHS making additional payments to us or require us to make payments to HHS.
We estimate and recognize adjustments to our health plan services premium revenue for the risk corridor
provision by projecting our ultimate premium for the calendar year. Such estimated calendar year amounts are
recognized ratably during the year and are revised each period to reflect current experience, including changes in risk
adjustment and reinsurance recoverables. We record receivables or payables and classify the amounts as current or long-
term in the consolidated balance sheets based on the timing of expected settlement. For the year ended December 31,
2014,we recorded $86.8 million of increases to risk corridor net receivable as health plan services premium revenue.
The risk corridor receivable balance included in other noncurrent assets as of December 31, 2014 was $90.4 million and
the risk corridor payable balance included in other noncurrent liabilities as of December 31, 2014 was $3.6 million.
HHS recognizes, in both final regulations and guidance, it is obligated to make the risk corridors program payments
without regard to budget neutrality. Although HHS anticipates the program will be budget neutral, the ACA requires
HHS to make full payments to those issuers with risk corridors ratios above 103 percent. Additionally, HHS states in
final regulations and guidance that if the program’s collections, including any potential carryover from prior years, are
insufficient to satisfy its payment obligations, the agency will use other sources of funding to meet its payment
obligations, subject to the availability of appropriations. If corridor collections are insufficient in 2014, HHS explains
that it shall fulfill its obligations for the 2014 benefit year by using funds collected for the 2015 benefit year prior to
making payments on 2015 obligations.
The final reconciliation and settlement with HHS of the premium and cost sharing subsidies and the amounts
related to the 3Rs for the current year will be completed in the following year with HHS.
Section 1202 of ACA
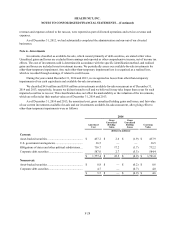
Section 1202 of the ACA mandates increases in Medicaid payment rates for primary care in calendar years 2013
and 2014. The final rule has been in effect since January 1, 2013. The provisions of section 1202 impact our 1.6 million
Medi-Cal members in California and 81,000 Medicaid members in Arizona. DHCS, the agency that regulates the Medi-
Cal program, initially implemented a reimbursement methodology with no underwriting risk to the managed care plans
("MCPs") in 2013. Subsequently, DHCS changed the reimbursement methodology during the second quarter of 2014,
and this change transferred full underwriting risk to the MCPs.
For the periods prior to this reimbursement methodology change, i.e., the year ended December 31, 2013 and the
three months ended March 31, 2014, we accounted for the provisions of section 1202 on an administrative services only
basis since it transferred no underwriting risk to the MCPs, and recorded the receipts and payments on a net basis.
Following the change in reimbursement methodology, we have full underwriting risk for 2013, including both
utilization and unit cost risk. Accordingly, for the year ended December 31, 2014, with respect to our Medi-Cal
business, we:
• Reversed $7.9 million previously recorded as administrative services fees and other income in 2013
and for the three months ended March 31, 2014.
• Recorded payments on a grossed-up basis by recording Medi-Cal payments received as premium
revenue and estimated Medi-Cal claim payments as health care costs (incurred claims), each via
retroactive adjustments to premium revenues and health care costs.
• Recorded retrospective premium revenue adjustments based upon the state settlement agreement (see
Note 2 - "Health Plan Services Revenue Recognition" above).