LabCorp 2013 Annual Report Download - page 23
Download and view the complete annual report
Please find page 23 of the 2013 LabCorp annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.19
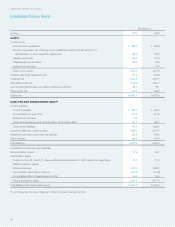
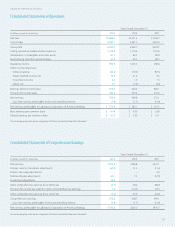
LABORATORY CORPORATION OF AMERICA
Management’s Discussion and Analysis
of Financial Condition and Results of Operations (in millions)
Forward-Looking Statements
The Company has made in this report, and from time to time may
otherwise make in its public filings, press releases and discussions
by Company management, forward-looking statements concerning
the Company’s operations, performance and financial condition, as
well as its strategic objectives. Some of these forward-looking state-
ments can be identified by the use of forward-looking words such
as “believes,” “expects,” “may,” “will,” “should,” “seeks,” “approximately,”
“intends,” “plans,” “estimates,” or “anticipates” or the negative of those
words or other comparable terminology. Such forward-looking
statements are subject to various risks and uncertainties and the
Company claims the protection afforded by the safe harbor for
forward-looking statements contained in the Private Securities
Litigation Reform Act of 1995. Actual results could differ materially
from those currently anticipated due to a number of factors in
addition to those discussed elsewhere herein and in the Company’s
other public filings, press releases and discussions with Company
management, including:
1. changes in federal, state, local and third-party payer regulations
or policies or other future reforms in the health care system
(or in the interpretation of current regulations), new insurance or
payment systems, including state, regional or private insurance
cooperatives (Health Insurance Exchanges), new public insur-
ance programs or a single-payer system, affecting governmental
and third-party coverage or reimbursement for clinical
laboratory testing;
2. significant monetary damages, fines, penalties, assessments,
refunds, repayments, and/or exclusion from Medicare and
Medicaid programs resulting from investigations, audits,
regulatory examinations, information requests, and other
inquiries by the government;
3. loss or suspension of a license or imposition of a fine or
penalties under, or future changes in, or interpretations of, the
law or regulations of the Clinical Laboratory Improvement
Act of 1967, and the Clinical Laboratory Improvement
Amendments of 1988, or those of Medicare, Medicaid, the
False Claims Act or other federal, state or local agencies;
4. penalties or loss of license arising from the failure to comply
with the Federal Occupational Safety and Health Administration
requirements and the Needlestick Safety and Prevention Act;
5. increased costs, denial of claims and/or significant penalties
arising from the failure to comply with HIPAA, including
changes to federal and state privacy and security obligations
and changes to HITECH and any subsequent amendments;
6. subsequent costs due to damage to the Company’s reputation
and significant litigation exposure arising from the failure to
maintain the security of business information or systems or
protect against cyber security attacks;
7. negative impact on the Company’s reimbursement, cash
collections, days sales outstanding and profitability arising from
the failure of the Company, third-party payers or physicians to
comply with the ICD-10-CM Code Set by the compliance date
of October 1, 2014;
8. increased competition, including competition from companies
that do not comply with existing laws or regulations or
otherwise disregard compliance standards in the industry;
9. increased price competition, competitive bidding for laboratory
tests and/or changes or reductions to fee schedules;
10. changes in payer mix, including an increase in capitated
reimbursement mechanisms or the impact of a shift to
consumer-driven health plans and adverse changes in payer
reimbursement or payer coverage policies related to specific
testing procedures or categories of testing;
11. failure to obtain and retain new customers or a reduction in
tests ordered or specimens submitted by existing customers;
12. failure to retain or attract managed care business as a result
of changes in business models, including new risk based or
network approaches, or other changes in strategy or business
models by managed care companies;
13. failure to effectively integrate and/or manage newly acquired
businesses and the cost related to such integrations;
14. adverse results in litigation matters;
15. inability to attract and retain experienced and
qualified personnel;