Humana 1999 Annual Report Download - page 14
Download and view the complete annual report
Please find page 14 of the 1999 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
workers’ compensation, Medicare supplement and North
Florida Medicaid businesses for proceeds of approximately
$115 million. The Company recorded a $118 million loss in
1999 related to these sale transactions.
On January 31, 2000, the Company acquired the Memorial
Sisters of Charity Health Network (“MSCHN”), a Houston
based health plan for approximately $50 million in cash.
On June 1, 1999, the Company reached an agreement with
FPA Medical Management, Inc. (“FPA”), FPA’s lenders and
a federal bankruptcy court under which the Company
acquired the operations of 50 medical centers from FPA for
approximately $14 million in cash. The Company has
subsequently reached agreements with 14 provider groups
to assume operating responsibility for 38 of the 50 acquired
FPA medical centers under long-term provider agreements
with the Company.
On October 17, 1997, the Company acquired ChoiceCare
Corporation (“ChoiceCare”) for approximately $250 million
in cash. The purchase was funded with borrowings under
the Company’s commercial paper program. ChoiceCare
provided health services products to members in the
Greater Cincinnati, Ohio, area.
On September 8, 1997, the Company acquired Physician
Corporation of America (“PCA”) for total consideration of
$411 million in cash, consisting primarily of $7 per share for
PCA’s outstanding common stock and the assumption of
$121 million in debt. The purchase was funded with
borrowings under the Company’s commercial paper
program. PCAprovided comprehensive health services
through its HMOs in Florida, Texas and Puerto Rico. In
addition, PCAprovided workers’ compensation third-party
administrative management services. Prior to November
1996, PCAalso was a direct writer of workers’
compensation insurance in Florida. Long-term medical and
other expenses payable in the accompanying Consolidated
Balance Sheets includes the long-term portion of workers’
compensation liabilities related to this business.
On February 28, 1997, the Company acquired Health Direct,
Inc. (“Health Direct”) from Advocate Health Care for
approximately $23 million in cash.
25
The consolidated financial statements of Humana Inc. (the
“Company” or “Humana”) in this Annual Report present
the Company’s financial position, results of operations and
cash flows, and should be read in conjunction with the
following discussion and analysis. This discussion and
analysis contains both historical and forward-looking
information. The forward-looking statements may be
significantly impacted by risks and uncertainties, and are
made pursuant to the safe harbor provisions of the Private
Securities Litigation Reform Act of 1995. There can be no
assurance that anticipated future results will be achieved
because actual results may differ materially from those
projected in the forward-looking statements. Readers are
cautioned that a number of factors, which are described
herein and in the Company’s Annual Report on Form 10-K
for the year ended December 31, 1999, could adversely
affect the Company’s ability to obtain these results. These
include the effects of either federal or state health care
reform or other legislation, including the Patients’ Bill of
Rights, any expanded right to sue managed care companies
and alleged class action litigation directed against the
managed care industry, changes in the Medicare
reimbursement system, the ability of health care providers
(including physician practice management companies) to
comply with current contract terms, renewal of the
Company’s Medicare contracts with the federal
government, renewal of the Company’s contract with the
federal government to administer the TRICARE program
and renewal of the Company’s Medicaid contracts with
various state governments and the Health Insurance
Administration in Puerto Rico. Such factors also include the
effects of other general business conditions, including but
not limited to, the success of the Company’s improvement
initiatives including its electronic business strategies,
premium rate and yield changes, retrospective premium
adjustments relating to federal government contracts,
changes in commercial and Medicare HMO membership,
medical and pharmacy cost trends, compliance with debt
covenants, changes in the Company’s debt rating and its
ability to borrow under its commercial paper program,
operating subsidiary capital requirements, competition,
general economic conditions and the retention of key
employees. In addition, past financial performance is not
necessarily a reliable indicator of future performance and
investors should not use historical performance to
anticipate results or future period trends.
I N T R O D U C T I O N
Humana is one of the nation’s largest publicly traded
health services companies that facilitates the delivery of
health care services through networks of providers to its
approximately 5.9 million medical members. The
Company’s products are marketed primarily through
health maintenance organizations (“HMOs”) and preferred
provider organizations (“PPOs”) that encourage or require
the use of contracted providers. HMOs and PPOs control
health care costs by various means, including pre-
admission approval for hospital inpatient services, pre-
authorization of outpatient surgical procedures, and
risk-sharing arrangements with providers. These providers
may share medical cost risk or have other incentives to
deliver quality medical services in a cost-effective manner.
The Company also offers various specialty products to
employers, including dental, group life and workers’
compensation and administrative services (“ASO”) to those
who self-insure their employee health plans. The Company
has entered into a definitive agreement to sell its workers’
compensation business. In total, the Company’s products
are licensed in 49 states, the District of Columbia and
Puerto Rico, with approximately 20 percent of its member-
ship in the state of Florida.
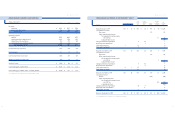
During 1999, the Company realigned its organization to
achieve greater accountability in its lines of business. As a
result of this realignment, the Company organized into two
business units: the Health Plan segment and the Small
Group segment. The Health Plan segment includes the
Company’s large group commercial (100 employees and
over), Medicare, Medicaid, ASO, workers’ compensation
and military or TRICARE business. The small group seg-
ment includes small group commercial (under 100 employ-
ees) and specialty benefit lines, including dental, life and
short-term disability. Results of each segment are measured
based upon results of operations before income taxes. The
Company allocates administrative expenses, interest income
and interest expense, but no assets, to the segments.
Members served by the two segments generally utilize the
same medical provider networks, enabling the Company to
obtain more favorable contract terms with providers. As
a result, the profitability of each segment is somewhat
interdependent. In addition, premium revenue pricing to
large group commercial employers has historically been
more competitive than that to small group commercial
employers, resulting in less favorable underwriting margins
for the large group commercial line of business. Costs to
distribute and administer products to small group
commercial employers are higher compared to large group
commercial employers resulting in small group’s higher
administrative expense ratio.
AC Q U I SI T IO NS AN D D I S P O S I T I O NS
Between December 30, 1999 and February 4, 2000, the
Company entered into definitive agreements to sell its
24
HU M A N A IN C .
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERAT I O N S
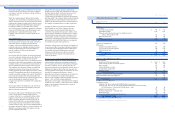
Selling, Asset
General and Write-Downs
(In millions) Medical Administrative and Other Total
1999:
FI R S T Q U A R T E R 1 9 9 9 :
Premium deficiency $ 50 $ 50
Reserve strengthening 35 35
Provider costs 5 5
Total first quarter 1999 90 90
F O U R T H Q UA RT ER 1 999 :
Long-lived asset impairment $ 342 342
Losses on non-core asset sales 118 118
Professional liability reserve strengthening and other costs $ 35 35
Total fourth quarter 1999 35 460 495
Total 1999 $ 90 $ 35 $ 460 $ 585
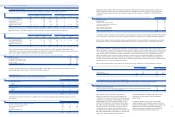
The above acquisitions were accounted for under the
purchase method of accounting. In connection with these
acquisitions, the Company allocated the acquisition costs to
net tangible and identifiable intangible assets based upon
their fair values. Identifiable intangible assets, which are
included in other long-term assets in the accompanying
Consolidated Balance Sheets, primarily relate to subscriber
and provider contracts. Any remaining value not assigned
to net tangible or identifiable intangible assets was then
allocated to cost in excess of net assets acquired, or
goodwill. Goodwill and identifiable intangible assets
acquired, recorded in connection with the acquisitions, was
$17 million and $754 million in 1999 and 1997, respectively.
Subscriber and provider contracts are amortized over their
estimated useful lives (seven to 14 years), while goodwill
has been amortized over periods from six to 40 years.
At December 31, 1999, goodwill and identifiable intangible
assets represent 67% of total stockholders’equity. In
accordance with the Company’s policy, the carrying values
of all long-lived assets including goodwill and identifiable
intangible assets are periodically reviewed by management
for impairment whenever adverse events or changes in
circumstances occur. In addition, management periodically
reviews the reasonableness of the estimated useful life
assigned to goodwill and identifiable intangible assets.
Impairment losses and/or changes in the estimated useful
life related to these assets could have a material adverse
impact on the Company’s financial position and results
of operations.
During 1999, the Company recorded an impairment loss
and, effective January 1, 2000, adopted a 20 year
amortization period from the date of acquisition for
goodwill previously amortized over 40 years as discussed
in the following section.
AS S E T W R IT E - DO W NS A N D O P E R AT I O NA L EX PE N SE S
The following table presents the components of the asset
write-downs and operational expenses and their respective
classifications in the 1999 and 1998 Consolidated Statements
of Operations: