Humana 1999 Annual Report Download - page 26
Download and view the complete annual report
Please find page 26 of the 1999 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
11 . A C Q U I S I T I O N S AN D D I S PO SI T IO NS
Between December 30, 1999 and February 4, 2000, the
Company entered into definitive agreements to sell its
workers’ compensation, Medicare supplement and North
Florida Medicaid businesses for proceeds of approximately
$115 million. The Company recorded a $118 million loss in
1999 related to these sale transactions.
On January 31, 2000, the Company acquired the Memorial
Sisters of Charity Health Network (“MSCHN”), a Houston
based health plan for approximately $50 million in cash.
On June 1, 1999, the Company reached an agreement with
FPA Medical Management, Inc. (“FPA”), FPA’s lenders and
a federal bankruptcy court under which the Company
acquired the operations of 50 medical centers from FPA for
approximately $14 million in cash. The Company has
subsequently reached agreements with 14 provider groups
to assume operating responsibility for 38 of the 50 acquired
FPA medical centers under long-term provider agreements
with the Company.
On October 17, 1997, the Company acquired ChoiceCare
Corporation (“ChoiceCare”) for approximately $250 million
in cash. The purchase was funded with borrowings under
the Company’s commercial paper program. ChoiceCare
provided health services products to members in the
Greater Cincinnati, Ohio, area.
On September 8, 1997, the Company acquired PCAfor total
consideration of $411 million in cash, consisting primarily
of $7 per share for PCA’s outstanding common stock and
the assumption of $121 million in debt. The purchase was
funded with borrowings under the Company’s commercial
paper program. PCAprovided comprehensive health
services through its HMOs in Florida, Texas and Puerto
Rico. In addition, PCAprovided workers’ compensation
third-party administrative management services. Prior to
November 1996, PCAalso was a direct writer of workers’
compensation insurance in Florida. Long-term medical and
other expenses payable in the accompanying Consolidated
Balance Sheets includes the long-term portion of workers’
compensation liabilities related to this business.
On February 28, 1997, the Company acquired Health Direct,
Inc. (“Health Direct”) from Advocate Health Care for
approximately $23 million in cash.
The above acquisitions were accounted for under the
purchase method of accounting. In connection with these
acquisitions, the Company allocated the acquisition costs to
net tangible and identifiable intangible assets based upon
their fair values. Identifiable intangible assets, which are
included in other long-term assets in the accompanying
Consolidated Balance Sheets, primarily relate to subscriber
and provider contracts. Any remaining value not assigned
to net tangible or identifiable intangible assets was then
allocated to cost in excess of net assets acquired, or
goodwill. Goodwill and identifiable intangible assets
acquired, recorded in connection with the acquisitions, was
$17 million and $754 million in 1999 and 1997, respectively.
Subscriber and provider contracts are amortized over their
estimated useful lives (seven to 14 years), while goodwill
has been amortized over periods from six to 40 years. After
a re-evaluation, effective January 1, 2000, the Company
adopted a 20 year amortization period from the date of
acquisition for goodwill previously amortized over
40 years.
The results of operations for the previously mentioned
acquisitions have been included in the accompanying
Consolidated Statements of Operations since the date of
acquisition. The following unaudited pro forma data
summarize the consolidated results of operations for the
year ended December 31, 1997 as if the 1997 acquisitions
referred to above had been completed as of the beginning
of 1997:
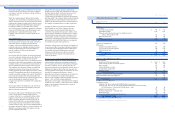
(In millions, except per share results)
Revenues $ 9,272
Net income 64
Earnings per common share $ 0.39
Earnings per common share — assuming dilution 0.39
The unaudited pro forma information above may not
necessarily reflect future results of operations or what the
results of operations would have been had the acquisitions
actually been consummated at the beginning of 1997.
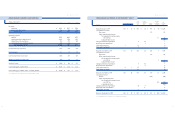
12 . S E G M EN T I N FO RM AT I O N
During 1999, the Company realigned its organization to
achieve greater accountability in its lines of business. As a
result of this realignment, the Company organized into two
business units: the Health Plan segment and the Small
Group segment. The Health Plan segment includes the
Company’s large group commercial (100 employees and
over), Medicare, Medicaid, ASO, workers’ compensation
and military or TRICARE business. The small group
segment includes small group commercial (under 100
employees) and specialty benefit lines, including dental, life
and short-term disability. Results of each segment are
measured based upon results of operations before income
taxes. The Company does not allocate assets to the
segments, but allocates administrative expenses, interest
income and interest expense to the segments. These
allocations are based on systematic and rational methods
which consider the nature of activities and volume of
business associated with the segments’ products. Members
served by the two segments generally utilize the same
medical provider networks, enabling the Company to
obtain more favorable contract terms with providers. As a
result, the profitability of each segment is somewhat
interdependent. In addition, premium revenue pricing to
large group commercial employers has historically been
more competitive than that to small group commercial
employers, resulting in less favorable underwriting margins
for the large group commercial line of business. Costs to
distribute and administer products to small group
commercial employers are higher compared to large group
commercial employers resulting in small group’s higher
administrative expense ratio. The accounting policies of
each segment are similar and are described in Note 2.
49
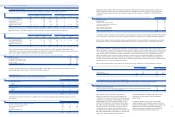
Future annual minimum payments under all noncancelable
operating leases in excess of one year subsequent to
December 31, 1999 are as follows:
(In millions)
2000 $ 54
2001 46
2002 31
2003 26
2004 22
Thereafter 62
Total minimum lease payments $ 241
Less: minimum sublease rental income (112)
Net minimum lease payments $ 129
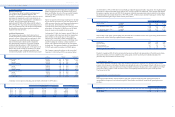
Government and Other Contracts
The Company’s Medicare HMO contracts with the federal
government are renewed for a one-year term each
December 31, unless terminated 90 days prior thereto.
Legislative proposals are being considered which may
revise the Medicare program’s current support of the use of
managed health care for Medicare beneficiaries and future
reimbursement rates thereunder. Management is unable to
predict the outcome of these proposals or the impact they
may have on the Company’s financial position, results of
operations or cash flows. The Company’s Medicaid con-
tracts are generally annual contracts with various states
except for the two-year contract with the Health Insurance
Administration in Puerto Rico. Additionally, the Company’s
TRICARE contract is a one-year contract renewable on July
1, 2000, for one additional year. The loss of these contracts
or significant changes in these programs as a result of
legislative action, including reductions in payments or
increases in benefits without corresponding increases in
payments, would have a material adverse effect on the
revenues, profitability and business prospects of the
Company. In addition, the Company continually contracts
and seeks to renew contracts with providers at rates
designed to ensure adequate profitability. To the extent the
Company is unable to obtain such rates, its financial
position, results of operations and cash flows could be
adversely impacted.
Legal Proceedings
During 1999, six purported class action complaints have
been filed against the Company and certain of its current
and former directors and officers claiming that the
Company and the individual defendants knowingly or
recklessly made false or misleading statements in press
releases and public filings concerning the Company’s
financial condition. All seek money damages of
unspecified amounts.
Since October 1999, the Company has received purported
class action complaints alleging, among other things, that
Humana intentionally concealed from its members
information concerning the various ways Humana decides
what claims will be paid, what procedures will be deemed
medically necessary, and what criteria and procedures are
used to determine the extent and type of their coverage.
The complaints also allege that Humana concealed from
members the existence of direct financial incentives to
treating physicians and other health care providers to deny
coverage. The complaints, generally, do not allege that any
member was denied coverage for services that should have
been covered but, instead, claim that Humana provided
health insurance benefits of lesser value than promised.
All seek money damages of unspecified amounts. The
Company has requested to consolidate these complaints to
a single court.
The Company believes the allegations in all of the above
complaints are without merit and intends to pursue the
defense of the actions vigorously.
On January 4, 2000, a jury in Palm Beach County, Florida,
issued a verdict against Humana Health Insurance
Company of Florida, Inc., awarding $79 million to Mark
Chipps, an insured who had sued individually and on
behalf of his minor daughter. The claim arose from the
removal of the child from a case management program
which had provided her with benefits in excess of those
available under her policy. The award included $78 million
for punitive damages, $1 million for emotional distress and
$28,000 for contractual benefits. The Company is in the
process of appealing the verdict.
During 1999, the Company reached an agreement in
principle with the United States Department of Justice and
the Department of Health and Human Services on a $15
million settlement relating to Medicare premium
overpayments. The settlement is expected to be paid
sometime during 2000. The Company had previously
established adequate liabilities for the resolution of these
issues and, therefore, the settlement did not have a material
impact on the Company’s financial position or results
of operations.
Damages for claims for personal injuries and medical
benefit denials are usual in the Company’s business.
Personal injury and medical benefit denial claims are
covered by insurance from the Company’s wholly owned
captive insurance Subsidiary and excess carriers, except to
the extent that claimants seek punitive damages, in states
which prohibit insurable coverage for punitive damages.
In connection with the Chipps case, the excess carriers have
preliminarily indicated that they believe no coverage may
be available for a punitive damages award.
During the ordinary course of its business, the Company is
or may become subject to pending or threatened litigation
or other legal actions. Management does not believe that
any pending and threatened legal actions against the
Company or audits by agencies will have a material
adverse effect on the Company’s financial position or
results of operations.
48
HU M A N A IN C .
NOTES TO CONSOLIDATED FINANCIAL STAT E M E N T S