LabCorp 2014 Annual Report Download - page 35
Download and view the complete annual report
Please find page 35 of the 2014 LabCorp annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.33
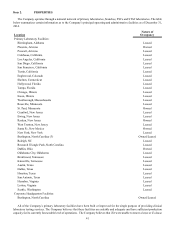
impact on the Company’s net revenues. For the year ended December 31, 2014, requisitions (based on the total volume of requisitions
excluding the Company's Other segment) by payer were:
• private patients – 1.3%
• Medicare and Medicaid – 14.4%
• commercial clients – 34.6%
• managed care – 49.7%
The various MCOs have different contracting philosophies, which are influenced by the design of the products they offer to
their members. Some MCOs contract with a limited number of clinical laboratories and engage in direct negotiation of the rates
reimbursed to participating laboratories. Other MCOs adopt broader networks with a generally largely uniform fee structure for
participating clinical laboratories. In addition, some MCOs have used capitation in an effort to fix the cost of laboratory testing
services for their enrollees. Under a capitated reimbursement mechanism, the clinical laboratory and the managed care organization
agree to a per member, per month payment to pay for all authorized laboratory tests ordered during the month by the physician
for the members, regardless of the number or cost of the tests actually performed. Capitation shifts the risk of increased test
utilization (and the underlying mix of testing services) to the clinical laboratory provider. The Company makes significant efforts
to ensure that its services are adequately compensated in its capitated arrangements. For the year ended December 31, 2014, such
capitated contracts accounted for approximately $211.1 million, or 3.7%, of the Company's net sales.
The Company's ability to attract and retain managed care clients is critical given the impact of health care reform, related
products and expanded coverage (e.g. Health Insurance Exchanges and Medicaid Expansion) and evolving delivery models (e.g.
Accountable Care Organizations).
A portion of the managed care fee-for-service revenues are collectible from patients in the form of deductibles, copayments
and coinsurance. As patient cost-sharing increases, collectibility may be impacted.
In addition, Medicare and Medicaid and private insurers have increased their efforts to control the cost, utilization and delivery
of health care services, including clinical laboratory services. Measures to regulate health care delivery in general, and clinical
laboratories in particular, have resulted in reduced prices, added costs and decreased test utilization for the clinical laboratory
industry by increasing complexity and adding new regulatory and administrative requirements. Pursuant to legislation passed in
late 2003, the percentage of Medicare beneficiaries enrolled in Medicare managed care plans has increased. The percentage of
Medicaid beneficiaries enrolled in Medicaid managed care plans has also increased, and is expected to continue to increase.
Implementation of the ACA, the health care reform legislation passed in 2010, also may affect coverage, reimbursement, and
utilization of laboratory services, as well as administrative requirements.
The Company also experienced delays in the pricing and implementation of new molecular pathology codes among various
payers, including Medicaid, Medicare and commercial carriers. While some delays were expected, several non-commercial payers
required an extended period of time to price key molecular codes and a number of those payers, mostly government entities,
indicated that they would no longer pay for tests that they had previously covered. Further, several payers are requiring additional
information to process claims or have implemented prior authorization policies. Many commercial payers were delayed in becoming
aware of the impact of their claim edits and policies which impeded access to services which previously have been covered and
reimbursed. These delays had a negative impact on 2014 revenue, revenue per requisition, margins and cash flows and are expected
to have a continuing negative impact. Similarly, coding changes related to toxicology and other procedures are being implemented
in 2015 and Palmetto has published a revised Drugs of Abuse Local Coverage Policy which, if implemented as written, would
adversely impact the Company's Medicare revenue. The policy has been delayed several times. It is currently published to be
effective April 1, 2015 and it is not clear what policies Medicaid and Managed Care organizations may implement in response.
The Company expects delays in the pricing and implementation of the new toxicology codes and it is unclear what impact will be
experienced related to price and margins.
The Company expects efforts to impose reduced reimbursement, more stringent payment policies and utilization and cost
controls by government and other payers to continue. If the Company cannot offset additional reductions in the payments it
receives for its services by reducing costs, increasing test volume and/or introducing new procedures, it could have a material
adverse impact on the Company’s net revenues, profitability and cash flows.
As an employer, health care reform legislation also contains numerous regulations that will require the Company to implement
significant process and record keeping changes to be in compliance. These changes increase the cost of providing health care
coverage to employees and their families. Given the limited release of regulations to guide compliance, the exact impact to
employers including the Company is uncertain.