Humana 2007 Annual Report Download - page 67
Download and view the complete annual report
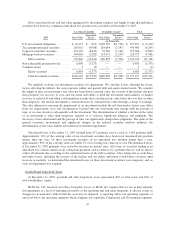
Please find page 67 of the 2007 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.government’s portion of prescription drug costs in the catastrophic layer of coverage. The capitation amount
represents a fixed monthly amount per member to provide prescription drug coverage in the catastrophic layer.
We chose the demonstration payment option for all of our enhanced benefit plans. This capitation amount,
derived from our annual bid submissions, is recorded as premium revenue. The variance between the capitation
amount and actual drug costs in the catastrophic layer is subject to risk sharing as part of the risk corridor
settlement.
Settlement of the reinsurance and low-income cost subsidies as well as the risk corridor payment is based on
a reconciliation made approximately 6 months after the close of each calendar year. This reconciliation process
requires us to submit claims data necessary for CMS to administer the program.
Medicare Risk Adjustment Provisions
CMS has implemented a risk adjustment model which apportions premiums paid to all health plans
according to health severity. The CMS risk adjustment model pays more for members with predictably higher
costs, as more fully described in Item 1.—Business on page 5. Under this risk adjustment methodology,
diagnosis data from inpatient and ambulatory treatment settings are used to calculate the risk adjusted premium
payment to us. We collect, capture, and submit the necessary and available diagnosis data to CMS within
prescribed deadlines. We estimate risk adjustment revenues based upon the diagnosis data submitted to CMS and
ultimately accepted by CMS. We do not have access to diagnosis data with respect to our stand-alone PDP
members.
CMS has transitioned to the risk adjustment model while the old demographic model was phased out. The
demographic model based the monthly premiums paid to health plans on factors such as age, sex and disability
status. The monthly premium amount for each member is separately determined under both the risk adjustment
and demographic model. These separate payment amounts are then blended according to the transition schedule.
CMS transitioned to the risk adjustment model for Medicare Advantage plans as follows: 30% in 2004, 50% in
2005, 75% in 2006, and 100% in 2007. The stand-alone PDP payment methodology is based 100% on the risk
adjustment model. As a result of this process and the phasing in of the risk adjustment model, as well as budget
neutrality as described in Item 1.—Business on page 5, our CMS monthly premium payments per member may
change materially, either favorably or unfavorably.
Military services
In 2007, military services revenues represented 12% of total premiums and administrative services fees.
Military services revenue primarily is derived from our TRICARE South Region contract with the Department of
Defense and in addition, beginning January 1, 2008, from our contract with the Department of Veterans Affairs.
Revenues associated with our contract with the Department of Veterans Affairs are recognized in the period
services are performed. The single TRICARE contract for the South Region includes multiple revenue generating
activities and as such was evaluated under Emerging Issues Task Force (EITF) Issue No. 00-21, Accounting for
Revenue Arrangements with Multiple Deliverables. We allocate the consideration to the various components
based on the relative fair values of the components. TRICARE revenues consist generally of (1) an insurance
premium for assuming underwriting risk for the cost of civilian health care services delivered to eligible
beneficiaries; (2) health care services provided to beneficiaries which are in turn reimbursed by the federal
government; and (3) administrative services fees related to claim processing, customer service, enrollment,
disease management and other services. We recognize the insurance premium as revenue ratably over the period
coverage is provided. Health care services reimbursements are recognized as revenue in the period health
services are provided. Administrative services fees are recognized as revenue in the period services are
performed.
The TRICARE contract contains provisions whereby the federal government bears a substantial portion of
the risk associated with financing the cost of health benefits. Annually, we negotiate a target health care cost
57