Humana 2003 Annual Report Download - page 113
Download and view the complete annual report
Please find page 113 of the 2003 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
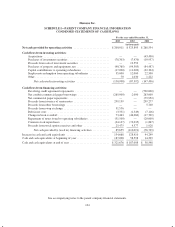
Humana Inc.
SCHEDULE I—PARENT COMPANY FINANCIAL INFORMATION
NOTES TO CONDENSED FINANCIAL STATEMENTS
1. BASIS OF PRESENTATION
Parent company financial information has been derived from our consolidated financial statements and
excludes the accounts of all operating subsidiaries. This information should be read in conjunction with our
consolidated financial statements.
2. TRANSACTIONS WITH SUBSIDIARIES
Management Fee
Through intercompany service agreements approved, if required, by state regulatory authorities, Humana
Inc., our parent company, charges a management fee for reimbursement of certain centralized services provided
to its subsidiaries including information systems, disbursement, investment and cash administration, marketing,
legal, finance, and medical and executive management oversight.
Dividends
Cash dividends received from subsidiaries and included as a component of net cash provided by operating
activities were $131.0 million in 2003 and $198.0 million in 2002. No cash dividends from subsidiaries were
received in 2001.
Guarantee
Through indemnity agreements approved by state regulatory authorities, certain of our regulated
subsidiaries generally are guaranteed by our parent company in the event of insolvency for; (1), member
coverage for which premium payment has been made prior to insolvency; (2), benefits for members then
hospitalized until discharged; and (3), payment to providers for services rendered prior to insolvency. Our parent
has also guaranteed the obligations of our TRICARE subsidiaries.
Notes Receivables from Operating Subsidiaries
We funded certain subsidiaries with surplus note agreements. These notes are generally non-interest bearing
and may not be repaid without the prior approval of the Departments of Insurance.
Notes Payable to Operating Subsidiaries
We borrowed funds from certain subsidiaries with notes generally collateralized by real estate. These notes,
which have various payment and maturity terms, bear interest ranging from 6.65% to 6.75% and are payable
between 2004 and 2009. We recorded interest expense of $3.9 million, $4.2 million and $5.2 million related to
these notes for the years ended December 31, 2003, 2002 and 2001, respectively.
3. REGULATORY REQUIREMENTS
Certain other subsidiaries operate in states that regulate the payment of dividends, loans or other cash
transfers to Humana Inc., require minimum levels of equity, and limit investments to approved securities. The
amount of dividends that may be paid to Humana Inc. by these subsidiaries, without prior approval by state
regulatory authorities, is limited based on the entity’s level of statutory income and statutory capital and surplus.
In most states, prior notification is provided before paying a dividend even if approval is not required.
As of December 31, 2003, we maintained aggregate statutory capital and surplus of an estimated $1,086.5
million in our state regulated health insurance subsidiaries. Each of these subsidiaries was in compliance with
applicable statutory requirements, which aggregated approximately $640.4 million.
105