Humana 2003 Annual Report Download - page 25
Download and view the complete annual report
Please find page 25 of the 2003 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
We view electronic submission as a favorable development that will simplify claims interactions. A few states
are considering proposals that place new limits on insurer contacts with hospitals and physicians. These
proposals include provisions to expand payment disclosure, limit implementation of claims payment procedures,
and extend an insurer payment liability where intermediaries fail to pay and restrict recoupment.
Some states are proposing the creation of small employer pooled purchasing arrangements. Although these
pooled purchasing arrangements may affect the small group market, most of the proposals require these
purchasing arrangements to comply with the standard small group market regulations. Similar arrangements
enacted in the early 1990s had a very limited affect on the small group insurance market. A limited number of
states are considering additional restrictions on the use of health status in small group rating. Mandate-free
benefit plans are pending in a number of states. Some of these proposals could allow insurers more flexibility in
the use of member cost sharing. There is activity in some states supporting an expansion of disclosure by
hospitals, physicians and other health care providers of quality and charge data either directly to patients or to
state agencies that must make it publicly available.
Medical malpractice reform is receiving significant attention. Pending medical malpractice reform proposals
differ substantially relative to the entities covered by the reforms. Since the substance of the reforms remains
under discussion and the scope of covered entities has not been resolved in most states, management is unable to
predict future activity under these laws.
We are unable to predict how existing federal or state laws and regulations may be changed or interpreted,
what additional laws or regulations affecting our businesses may be enacted or proposed, when and which of the
proposed laws will be adopted or what effect any such new laws and regulations will have on our financial
position, results of operations or cash flows.
Other
Captive Insurance Company
We bear general business risks associated with operating our Company such as professional and general
liability, employee workers’ compensation, and officer and director errors and omissions risks. Professional and
general liability risks may include, for example, medical malpractice claims and disputes with members
regarding benefit coverage. We retain these risks through our wholly-owned, consolidated insurance subsidiary.
We reduce exposure to our own general business risks by insuring levels of coverage for losses in excess of our
retained limits with a number of third party insurance companies. We remain liable in the event these insurance
companies are unable to pay their portion of the losses. In an effort to minimize credit risk, we insure our risks
with a number of insurance companies having a long history of strong financial ratings. On January 1, 2002, and
again on January 1, 2003, we reduced the amount of coverage purchased from third party insurance carriers and
increased the amount of risk we retain due to substantially higher insurance rates. We provide a detail of the
significant assets and liabilities related to our captive insurance subsidiary in Note 9 to the consolidated financial
statements.
Centralized Management Services
We provide centralized management services to each health plan from our headquarters and service centers.
These services include management information systems, product administration, financing, personnel,
development, accounting, legal advice, public relations, marketing, insurance, purchasing, risk management,
actuarial, underwriting, and claims processing.
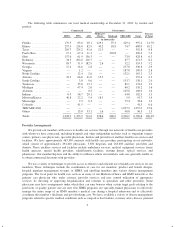
Employees
As of December 31, 2003, we had approximately 13,700 employees. We have not experienced any work
stoppages and believe we have good relations with our employees.
17