Humana 2003 Annual Report Download - page 15
Download and view the complete annual report
Please find page 15 of the 2003 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
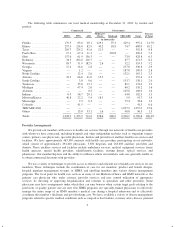
approximately 5% for the five-year period beginning January 1, 2000. Over the last several years, our
Medicare+Choice membership has declined as we exited some counties. These exits were a result, in part, of
lower CMS reimbursement rates.
In December 2003, the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, or
DIMA was signed into law. The legislation establishes a new Medicare private health plan program, called
MedicareAdvantage, continuing the health plan options afforded under the former Medicare+Choice program
while adding additional health plan options, including regional PPO options beginning in 2006. DIMA includes
provisions that require the 2004 stabilization funding to be directed toward increased reimbursement for
providers, increased benefits or access for members, or decreased member premiums. Including DIMA funding
and changes in member premiums, we expect an 8% to 10% increase in total per member premiums in 2004 with
a corresponding increase in medical costs due to increased reimbursements for providers and increased benefits
for members.
Medicaid Product
Medicaid is a federal program that is state-operated to facilitate the delivery of health care services to low-
income residents. Each electing state develops, through a state specific regulatory agency, a Medicaid managed
care initiative that must be approved by CMS. CMS requires that Medicaid managed care plans meet federal
standards and cost no more than the amount that would have been spent on a comparable fee-for-service basis.
States currently either use a formal proposal process in which they review many bidders before selecting one or
award individual contracts to qualified bidders who apply for entry to the program. In either case, the contractual
relationship with a state generally is for a one-year period. Under these contracts, we receive a fixed monthly
payment from a government agency for which we are required to provide health insurance coverage to enrolled
members. Due to the increased emphasis on state health care reform and budgetary constraints, more states are
utilizing a managed care product in their Medicaid programs.
We currently have Medicaid contracts with the Puerto Rico Health Insurance Administration through June
30, 2005, subject to each party agreeing upon annual rates. In July 2003, we signed amendments to the Puerto
Rico Medicaid contracts regarding a premium rate increase for the annual period ending June 30, 2004. Our other
Medicaid contracts are in Florida and Illinois, and are annual contracts. For the year ended December 31, 2003,
premium revenues from our Medicaid products totaled $487.1 million, or 4.0% of our total premiums and ASO
fees. At December 31, 2003, we had approximately 394,800 Medicaid members in Puerto Rico, or 84% of total
Medicaid members, and 74,100 Medicaid members in Florida and Illinois, or 16% of total Medicaid members.
TRICARE
TRICARE provides health insurance coverage to the dependents of active duty military personnel and to
retired military personnel and their dependents. In November 1995, the United States Department of Defense
awarded us our first TRICARE contract for Regions 3 and 4 covering approximately 1.1 million eligible
beneficiaries in Florida, Georgia, South Carolina, Mississippi, Alabama, Tennessee and Eastern Louisiana. On
July 1, 1996, we began providing health insurance coverage to these approximately 1.1 million eligible
beneficiaries.
On May 31, 2001, we purchased the entity responsible for administering TRICARE benefits for Regions 2
and 5 to approximately 1.2 million eligible beneficiaries in Illinois, Indiana, Kentucky, Michigan, North
Carolina, Ohio, Tennessee, Virginia, Wisconsin, West Virginia and a portion of Missouri.
Our current TRICARE contract with the Department of Defense will be in effect until April 30, 2004 for
Regions 2 and 5 and until June 30, 2004 for Regions 3 and 4. Each of the contracts is subject to a one-year
renewal at the Government’s option. We believe these contracts will continue until the TRICARE transition
described below.
7