Humana 2005 Annual Report Download - page 16
Download and view the complete annual report
Please find page 16 of the 2005 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
payment model. The payment adjustments for budget neutrality were first developed in 2002 and began to be
used with the 2003 payments.
The budget neutrality adjustment will begin phasing out in 2007 and will be fully eliminated by 2011. This
does not mean, however, that the aggregate per-member payments to Medicare plans will be reduced. As plans
enroll less healthy beneficiaries, the need for the budget neutrality adjustment declines as the underlying risk
adjusted Medicare rates paid to plans increase to account for their enrollees’ greater healthcare needs. As a result
of changes in the CMS payment processes, including the phasing in of the risk adjustment methodology and the
phasing out of the budget neutrality adjustment described previously, our CMS payments per member may
change materially, either favorably or unfavorably.
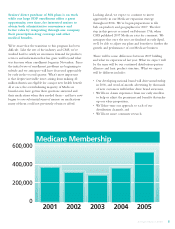
At December 31, 2005, we provided health insurance coverage under CMS contracts to approximately
557,800 Medicare Advantage members for which we received premium revenues of approximately $4.6 billion,
or 32.2% of our total premiums and ASO fees for the year ended December 31, 2005. Under our contracts with
CMS in Florida, we provided health insurance coverage to approximately 295,400 members. These contracts
accounted for premium revenues of approximately $2.8 billion, which represented approximately 60.9% of our
Medicare Advantage premium revenues, or 19.9% of our total premiums and ASO fees for the year ended
December 31, 2005.
Our HMO, PPO and PFFS products covered under Medicare Advantage contracts with CMS are renewed
generally for a one-year term each December 31 unless CMS notifies Humana of its decision not to renew by
May 1 of the contract year, or Humana notifies CMS of its decision not to renew by the first Monday in June of
the contract year.
Medicare Prescription Drug Products
On January 1, 2006, we began covering members in prescription drug plans, or PDPs, under Medicare Part
D. For 2006 coverage, Medicare-eligible individuals may enroll between November 15, 2005 and May 15, 2006
in one of our three plan choices. These three plan choices, Standard, Enhanced and Complete, may vary in terms
of coverage levels and out-of-pocket costs for premiums, deductibles and co-insurance with the Standard plan
offering the minimum benefits mandated by Congress. Our bid amount generally represents the payment we
receive from CMS. However, this payment is subject to adjustments and subsidies in order for Humana and CMS
to share the risk associated with financing the ultimate cost of the health benefit. Further, the amount of the
payment we receive from CMS is subject to the risk adjustment payment process previously described in order to
take into account beneficiaries’ health status risk factors. Unlike our Medicare Advantage products, there is no
phase-in of the risk adjustment payment process for our PDP products. Our PDP products covered under
Medicare Part D contracts with CMS are renewed generally for a one-year term each December 31 unless CMS
notifies Humana of its decision not to renew by May 1 of the contract year, or Humana notifies CMS of its
decision not to renew by the first Monday in June of the contract year.
Medicare Presence
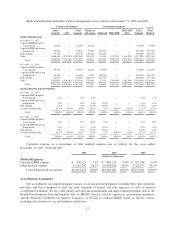
The following table sets forth the number of markets in which we sold our Medicare Advantage and PDP
products as of January 1, 2006, as compared with January 1, 2005 and 2004:
2006 2005 2004
HMO (localities) .......................................... 12 12 11
Local PPO (localities) ...................................... 33 30 1
Regional PPO (states) ...................................... 23 — —
PFFS (states) ............................................. 35 35 12
PDP (states) .............................................. 46 — —
In addition, we are marketing our HMO and PFFS products in Puerto Rico for coverage beginning
January 1, 2006.
6