Humana 2005 Annual Report Download - page 99
Download and view the complete annual report
Please find page 99 of the 2005 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Humana Inc.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
persons enrolled or eligible to enroll due to the federal government’s decision to increase or decrease U.S.
military presence around the world. In the event government reimbursements were to decline from projected
amounts, our failure to reduce the health care costs associated with these programs could have a material adverse
effect on our business.
Our Medicaid business, which accounted for approximately 4% of our total premiums and ASO fees for the
year ended December 31, 2005, consisted of contracts in Puerto Rico, Florida and Illinois. Our 3-year contracts
with the Puerto Rico Health Insurance Administration, which accounted for approximately 3% of our total
premium and ASO fees for the year ended December 31, 2005, were extended a fourth year and these contracts
expire on June 30, 2006. We are preparing to bid on the new contracts that will be effective July 2006 although a
request for such proposal has not yet been issued by the Puerto Rico Health Insurance Administration. At this
time we are unable to predict the ultimate impact that any government policy decisions might have on our
Medicaid contracts in Puerto Rico.
Our other current Medicaid contract, which is in Florida, is scheduled to expire on June 30, 2006. Due to
Medicaid reform in Florida, we are currently negotiating the terms and rates for the renewal contract. We expect
the current contract to be extended until August 31, 2006, and the subsequent renewal contract to be effective for
a two-year term beginning September 1, 2006. Due to continual decreases in the reimbursement from the state of
Illinois, we exited the Illinois Medicaid market effective July 31, 2005. The Illinois and Florida Medicaid
contracts accounted for approximately 1% of our total premiums and ASO fees for the year ended December 31,
2005.
Other than as described herein, the loss of any of the contracts above or significant changes in these
programs as a result of legislative action, including reductions in premium payments to us, or increases in
member benefits without corresponding increases in premium payments to us, may have a material adverse effect
on our financial position, results of operations, and cash flows.
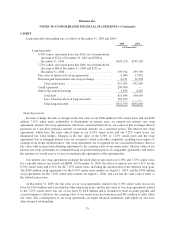
Legal Proceedings
Managed Care Industry Purported Class Action Litigation
Since 1999, we have been involved in several purported class action lawsuits that were part of a wave of
generally similar actions targeting the health care payer industry and particularly managed care companies. These
included a lawsuit against us and originally nine of our competitors that purported to be brought on behalf of
physicians who treated our members since January 1, 1990. The plaintiffs asserted that we and other defendants
paid providers’ claims incorrectly by paying lesser amounts than they submitted. These cases were consolidated
in the United States District Court for the Southern District of Florida (“the Court”), and styled In re Managed
Care Litigation.
On October 17, 2005, we and representatives of over 700,000 physicians and several state medical societies
reached an agreement (“Settlement Agreement”) to settle the lawsuit by payment of $40 million for the
physicians and an amount up to $18 million for the plaintiffs’ attorneys, subject to approval by the Court. The
Settlement Agreement recognizes that we have undertaken certain initiatives to facilitate relationships with, and
payments to, physicians and provides for additional initiatives over its four-year term. The Court preliminarily
approved the Settlement Agreement on October 19, 2005, and set a Settlement Hearing for March 6, 2006.
Three other defendants, Aetna Inc., Cigna Corporation, and The Prudential Insurance Company of America
previously entered into settlement agreements that have been approved by the Court. Health Net, Inc. announced
a settlement agreement on May 2, 2005, and Wellpoint, Inc. (formerly WellPoint Health Networks, Inc. and
Anthem, Inc.) announced a settlement agreement on July 11, 2005.
89