Humana 2005 Annual Report Download - page 18
Download and view the complete annual report
Please find page 18 of the 2005 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.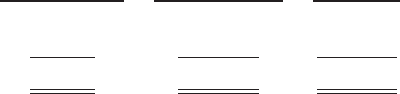
cost amount could have a material adverse effect on our business. These changes may include, for example, an
increase or reduction in the number of persons enrolled or eligible to enroll due to the federal government’s
decision to increase or decrease U.S. military presence around the world. In the event government
reimbursements were to decline from projected amounts, our failure to reduce the health care costs associated
with these programs could have a material adverse effect on our business.
During 2004, we completed a contractual transition of our TRICARE business. On July 1, 2004, our
Regions 2 and 5 contract servicing approximately 1.1 million TRICARE members became part of the new North
Region, which was awarded to another contractor. On August 1, 2004, our Regions 3 and 4 contract became part
of our new South Region contract. On November 1, 2004, the Region 6 contract with approximately 1 million
members became part of the South Region contract. The members added with the Region 6 contract essentially
offset the members lost four months earlier with the expiration of our Regions 2 and 5 contract. For the year
ended December 31, 2005, TRICARE premium revenues were approximately $2.4 billion, or 16.9% of our total
premiums and ASO fees.
Part of the TRICARE transition during 2004 included the carve out of the TRICARE Senior Pharmacy and
TRICARE for Life program which we previously administered on as ASO basis. On June 1, 2004 and August 1,
2004, administrative services under these programs were transferred to another contractor. For the year ended
December 31, 2005, TRICARE administrative services fees totaled $50.1 million, or 0.4% of our total premiums
and ASO fees.
Our Products Marketed to Commercial Segment Employers and Members
Consumer-Choice Products
Over the last several years, we have developed and offered various commercial products designed to
provide options and choices to employers that are annually facing substantial premium increases driven by
double-digit medical cost inflation. These consumer-choice products, which can be offered on either a fully
insured or ASO basis, provided coverage to approximately 371,100 members at December 31, 2005, representing
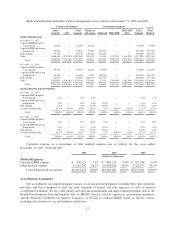
approximately 11.7% of our total commercial medical membership as detailed below.
Consumer-Choice
Membership
Other Commercial
Membership
Commercial
Medical
Membership
Fully insured ..................... 184,000 1,815,800 1,999,800
Administrative services only ......... 187,100 983,900 1,171,000
Total Commercial medical ...... 371,100 2,799,700 3,170,800
These products are often offered to employer groups as “bundles”, where the subscribers are offered various
HMO and PPO options, with various employer contribution strategies as determined by the employer.
Paramount to our consumer-choice product strategy, we have developed a group of innovative consumer
products, styled as “Smart” products, that we believe will be a long-term solution for employers. We believe this
new generation of products provides more (1) choices for the individual consumer, (2) transparency of provider
costs, and (3) benefit designs that engage consumers in the costs and effectiveness of health care choices.
Innovative tools and technology are available to assist consumers with these decisions, including the trade-offs
between higher premiums and point-of-service costs at the time consumers choose their plans, and to suggest
ways in which the consumers can maximize their individual benefits at the point they use their plans. We believe
that when consumers can make informed choices about the cost and effectiveness of their health care, a
sustainable long term solution for employers can be realized. Smart products, which accounted for approximately
65.1% of enrollment in all of our consumer-choice plans as of December 31, 2005, only are sold to employers
who use Humana as their sole health insurance carrier.
8