Humana 2002 Annual Report Download
Download and view the complete annual report
Please find the complete 2002 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
ANNUAL REPORT 2002
A Health Benefits Company
Guidance when you need it most
Table of contents
-
Page 1
ANNUAL REPORT 2002 Guidance when you need it most A H e a l t h B e n e f i t s C o m p a n y -
Page 2
...health care system Michael B. McCallister, Director, President and Chief Executive Officer (left) David A. Jones, Chairman of the Board (right) that seems like an impenetrable maze, Humana in 2002 began offering innovative products and product support that combine the best of traditional health plan... -
Page 3
... a PlanWizard during the selection process, a personalized home page and fast access to Webbased customer service. CoverageFirst features reduced premiums for consumers. It offers a basic layer of first-dollar coverage, $500 per member, supplied by the employer through the plan. The next layer is... -
Page 4
... segments were additive to our membership this year, as Commercial segment sales increased for the first time in several years, and the number of beneficiaries eligible for the TRICARE program expanded. Our medical expense ratio (medical expenses as a percent of premiums) was 83.6 percent in 2002... -
Page 5
...as a health benefits company committed to growth through innovation, we're well positioned to address that dilemma with a proven solution to meet a broad marketplace demand. Sincerely, David A. Jones Chairman of the Board Significant stockholder Michael B. McCallister Director, President and Chief... -
Page 6
... $ $ Humana Inc., headquartered in Louisville, Kentucky, is one of the nation's largest publicly traded health benefits companies, with approximately 6.6 million medical members located primarily in 18 states and Puerto Rico. Humana offers coordinated health insurance coverage and related services... -
Page 7
... period from to Commission file number 1-5975 (Exact name of registrant as specified in its charter) HUMANA INC. Delaware (State of incorporation) 61-0647538 (I.R.S. Employer Identification Number) 500 West Main Street Louisville, Kentucky (Address of principal executive offices) 40202 (Zip... -
Page 8
HUMANA INC. INDEX TO ANNUAL REPORT ON FORM 10-K For the Year Ended December 31, 2002 Page Part I Item 1. Item 2. Item 3. Item 4. Business ...Properties ...Legal Proceedings ...Submission of Matters to a Vote of Security Holders ...Part II Item 5. Item 6. Item 7. Item 7a. Item 8. Item 9. Market for ... -
Page 9
... specialty products programs. We have approximately 425,000 contracts with physicians, hospitals, dentists and other providers to provide health care to our members. In 2002, approximately 70% of our premiums and administrative services fees resulted from members located in Florida, Illinois, Texas... -
Page 10
... Commercial segment profitability focuses on providing solutions for employers to the rising cost of health care through the use of innovative and consumer-centric product designs which are supported by service excellence and industry-leading electronic capabilities, including education, tools... -
Page 11
... form of managed care. An HMO member, typically through the member's employer, pays a monthly fee, which generally covers, with some copayments, health care services received from or approved by the member's primary care physician. For the year ended December 31, 2002, commercial HMO premium... -
Page 12
... required to pay a premium to the federal government, which is adjusted annually, to be eligible for physician care and other services, known as Part B care. We contract with CMS under the Medicare+Choice program to provide health insurance coverage in exchange for a fixed monthly payment per member... -
Page 13
... formed Anthem Alliance Health Insurance Company subsidiary responsible for administering TRICARE benefits for Regions 2 and 5 to approximately 1.2 million eligible members in Illinois, Indiana, Kentucky, Michigan, a portion of Missouri, North Carolina, Ohio, Tennessee, Virginia, Wisconsin and West... -
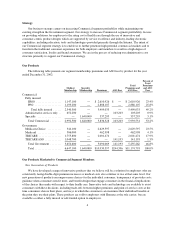
Page 14
... our medical membership at December 31, 2002, by market and product: Commercial HMO PPO ASO Government Medicare + Choice Medicaid TRICARE (in thousands) Percent Of Total Total Florida ...Illinois ...Texas ...Puerto Rico ...Ohio ...Kentucky ...Wisconsin ...Georgia ...Virginia ...North Carolina... -
Page 15
..., product and benefit designs, hospital inpatient management systems, or HIMS, and enrolling members into various disease management programs. The focal point for health care services in many of our Medicare+Choice and HMO networks is the primary care physician who, under contract, provides services... -
Page 16
...: Commercial Segment Fully Insured ASO Total Segment Medicare+ Choice Government Segment Medicaid TRICARE TRICARE ASO Total Segment Consol. Total Medical Medical Membership: December 31, 2002 Capitated HMO hospital system based ...147,400 Capitated HMO physician group based ...73,900 Risk-sharing... -
Page 17
... for health plan standards in quality management, credentialing, rights and responsibilities, and network management. Seven markets have achieved URAC health plan accreditation for all HMO product lines: Humana Medical Plan, Inc. in north Florida, south Florida, central Florida (Daytona, Tampa and... -
Page 18
...health plans in the markets in which we compete. Our ability to sell our products and to retain customers is, or may be, influenced by such factors as benefits, pricing, contract terms, number and quality of participating physicians and other managed health care providers, utilization review, claims... -
Page 19
... 2003, Humana Medical Plan, Inc., Humana Health Plan of Texas, Inc., and Humana Health Plan, Inc. each hold CMS contracts under the Medicare+Choice program to sell Medicare HMO products in a total of six states. In addition, Humana Insurance Company holds a CMS contract under a Medicare+Choice pilot... -
Page 20
...utilization review procedures, quality assurance, complaint systems, enrollment requirements, claim payments, marketing and advertising. The HMO, PPO and other health insurance-related products we offer are sold under licenses issued by the applicable insurance regulators. Under state laws, our HMOs... -
Page 21
... benefits are provided through insurance products or are self-funded. As a result, the new claims and appeals review regulation impacts nearly all employer and union-sponsored health and disability plans, except church and government plans. Similar to legislation recently passed by many states... -
Page 22
... to reduce the number of medical errors by health care providers and systems of care, and various state and federal purchasing plans to allow individuals and small employers to purchase health insurance. Also, Congress is evaluating proposals to expand Medicare benefits to cover prescription drugs... -
Page 23
...The following table lists the location of properties we owned or leased at December 31, 2002: Medical Centers Owned Leased Administrative Offices Owned Leased Total Florida ...Kentucky ...Illinois ...Texas ...Georgia ...North Carolina ...Ohio ...Puerto Rico ...Wisconsin ...Missouri/Kansas ...Others... -
Page 24
...Organizations Act, or RICO, for all persons who are or were subscribers at any time during the four-year period prior to the filing of the complaints. Plaintiffs also seek to represent a subclass of policyholders who purchased insurance through their employers' health benefit plans governed by ERISA... -
Page 25
...subclass consists of medical doctors who provided services to any person insured in California by any defendant when the doctor was not bound to arbitrate the claim. On October 10, 2002, the defendants asked the Court of Appeals for the Eleventh Circuit to review the class certification decision. On... -
Page 26
... we entered into a five-year Corporate Integrity Agreement, or CIA, with the Office of Inspector General, or OIG, of the Department of Health and Human Services. Under the CIA, we are obligated to, among other things, provide training, conduct periodic audits and make periodic reports to the OIG. In... -
Page 27
... STOCKHOLDER MATTERS Market Information Our common stock trades on the New York Stock Exchange under the symbol HUM. The following table shows the range of high and low closing sales prices as reported on the New York Stock Exchange Composite Tape for each quarter in the years ended December 31... -
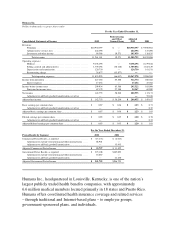
Page 28
... 6. SELECTED FINANCIAL DATA 2002 (a)(b) 2001 2000 1999 (c) 1998 (d) (in thousands, except per share results, membership and ratios) Summary of Operations Revenues: Premiums ...Administrative services fees ...Investment and other income ...Total revenues ...Operating expenses: Medical ...Selling... -
Page 29
... federal government contract with the Centers for Medicare and Medicaid Services, or CMS, we provide health insurance coverage to approximately 228,400 Medicare+Choice members in Florida, accounting for approximately 16% of our total premiums and administrative services fees in 2002. We manage our... -
Page 30
... including customer service, claim administrations, clinical operations, provider network administration, as well as other corporate and fieldbased positions. As part of the plan, we expect to hire approximately 300 employees to support newly consolidated operations, thereby resulting in a net... -
Page 31
...incurred to provide health insurance coverage to members, as well as estimates of future payments to hospitals and others for medical care provided prior to the balance sheet date. Capitation payments represent monthly contractual fees disbursed to primary care physicians and other providers who are... -
Page 32
.... Administrative services fees cover the processing of claims, offering access to our provider networks and clinical programs, and responding to customer service inquiries from members of self-funded employers. Under ASO contracts, selffunded employers and, for TRICARE ASO, the Department of Defense... -
Page 33
... provider networks, same-store utilization of services and administrative overhead. However, the federal government retains the financial risk associated with changes in usage levels at military treatment facilities, or MTF, changes in the number of persons eligible for TRICARE benefits and medical... -
Page 34
..., comparing the security with securities of publicly traded companies in a similar line of business, and reviewing the underlying financial performance including estimating discounted cash flows. Unrealized holding gains and losses, net of applicable deferred taxes, are included as a component... -
Page 35
...outstanding shares of common stock of a newly-formed Anthem Health Insurance Company subsidiary responsible for administering TRICARE benefits in Regions 2 and 5 for $43.5 million in cash, net of direct transaction costs. During 2000, in separate transactions, we acquired a Houston-based health plan... -
Page 36
... additional disclosure in filings issued after January 31, 2003. The adoption of FIN 46 is not expected to have a material impact on our financial position, results of operations or cash flows. In January 2003, the FASB issued Statement No. 148, Accounting for Stock-Based Compensation- Transition... -
Page 37
... year ended December 31, 2002 2001 (in thousands, except ratios) Premium revenues: Fully insured ...$ 5,499,033 Specialty ...337,295 Total Commercial ...Medicare+Choice ...TRICARE ...Medicaid ...Total Government ...Total ...Administrative services fees: Commercial ...Government ...Total ...Medical... -
Page 38
... 31, 2002 2001 Change Members Percentage Commercial segment medical members: Fully insured ...2,340,300 ASO ...652,200 Total Commercial ...Government segment medical members: Medicare+Choice ...Medicaid ...TRICARE ...TRICARE ASO ...Total Government ...Total medical membership ...2,992,500 344,100... -
Page 39
...attributable to the implementation of the TRICARE for Life benefits program effective October 1, 2001. TRICARE for Life is a program for seniors where we provide medical benefit administrative services. Investment and Other Income Investment and other income totaled $86.4 million in 2002, a decrease... -
Page 40
... generated from administrative services fees, primarily from the TRICARE Regions 2 and 5 acquisition and the implementation of the TRICARE for Life benefit programs effective October 1, 2001, as discussed above. ASO business carries a much higher SG&A ratio than fully insured business. We expect... -
Page 41
... year ended December 31, 2001 2000 (in thousands, except ratios) Premium revenues: Fully insured ...$4,941,888 Specialty ...304,714 Total Commercial ...Medicare+Choice ...TRICARE ...Medicaid ...Total Government ...Total ...Administrative services fees: Commercial ...Government ...Total ...Medical... -
Page 42
... of our north Florida, Milwaukee, Wisconsin, and Austin, San Antonio and Houston, Texas Medicaid businesses. For 2001, TRICARE premiums were $1.3 billion compared to $892.4 million for 2000, an increase of $449.2 million. Fully insured TRICARE membership increased by 644,300 members, or 60... -
Page 43
... fees for 2001 were $137.1 million, an increase of $50.8 million from $86.3 million for 2000. This increase primarily was due to the TRICARE Regions 2 and 5 acquisition, and servicing medical benefits in an administrative capacity under a new TRICARE program for seniors, called TRICARE for Life... -
Page 44
... benefit of capital loss carryforwards resulting from the sale of our workers' compensation business. Liquidity The following table presents operating cash flows for the years ended December 31, 2002 and 2001, excluding the effects of the timing of the Medicare+Choice premium receipts: For the years... -
Page 45
...to the billing and enrollment system. Capital Expenditures Our ongoing capital expenditures relate primarily to our technology initiatives and administrative facilities necessary for activities such as claims processing, billing and collections, medical utilization review and customer service. Total... -
Page 46
...the credit agreement to a one year term loan upon expiration. The 4-year revolving credit agreement expires in October 2005. In October 2002, we renewed the 364-day revolving credit agreement which expires in October 2003, unless extended. There were no balances outstanding under either agreement at... -
Page 47
... compliance assuming the more restrictive future financial covenant requirements were applicable at December 31, 2002. Commercial Paper Programs We maintain indirect access to the commercial paper market through our conduit commercial paper financing program. Under this program, a third party issues... -
Page 48
... approved by the state regulatory authorities, certain of our regulated subsidiaries generally are guaranteed by Humana Inc., our parent company, in the event of insolvency for (1) member coverage for which premium payment has been made prior to insolvency; (2) benefits for members then hospitalized... -
Page 49
... number of years. If RBC were fully implemented by all states at December 31, 2002, each of our subsidiaries would be in compliance, and we would have $358.8 million of aggregate capital and surplus above the minimum level required under RBC. One TRICARE subsidiary under the Regions 3 and 4 contract... -
Page 50
... with the Department of Defense to extend our TRICARE contracts that expire on April 30, 2003 for Regions 2 and 5 and June 30, 2003 for Regions 3 and 4. We believe we will be able to successfully extend our TRICARE contracts under substantially the same terms for one additional year plus a 44 -
Page 51
... 86% of our total Medicaid membership as of December 31, 2002. The term of each of these contracts is three years, subject to annual renewal options with the Health Insurance Administration in Puerto Rico. Our Medicaid contracts in Florida and Illinois generally are annual contracts. The loss of... -
Page 52
... centralized expenses and various other costs incurred to provide health insurance coverage to our members. These costs also include estimates of future payments to hospitals and others for medical care provided to our members. Generally, premiums in the health care business are fixed for one-year... -
Page 53
... to the challenge of controlling health care costs, we face competitive pressure to contain premium prices. Premium increases, introduction of new product designs, and our relationship with our providers in various markets, among others, could affect our membership levels. Other actions that could... -
Page 54
..., results of operations and cash flows; at December 31, 2002, under one of our CMS contracts, we provided health insurance coverage to approximately 228,400 members in Florida. This contract accounted for approximately 16% of our total premiums and ASO fees for the year ended December 31, 2002... -
Page 55
... to minimum net worth; licensing requirements; approval of policy language and benefits; mandated benefits and processes; provider compensation arrangements; member disclosure; premium rates; and periodic examinations by state and federal agencies. State regulations require our licensed, operating... -
Page 56
... medical necessity; health insurance access; provider compensation and contract language; disclosure of provider fee schedules and other data impacting payments to providers; health plan liability to members who fail to receive appropriate care; disclosure and composition of physician networks... -
Page 57
... benefits are provided through insurance products or are self-funded. As a result, the new claims and appeals review regulation impacts nearly all employer and union-sponsored health and disability plans, except church and government plans. Similar to legislation recently passed by many states... -
Page 58
.... One TRICARE subsidiary under the Regions 3 and 4 contract with the Department of Defense is required to maintain assets at least equivalent to its current liabilities. In addition, we normally notify the state departments of insurance prior to making payments that do not require approval. ITEM... -
Page 59
...,833 Receivables, less allowance for doubtful accounts of $30,178 in 2002 and $38,539 in 2001 ...Premiums ...348,562 Administrative services fees ...68,316 Other ...250,857 Total current assets ...2,794,925 Property and equipment, net ...459,842 Other assets: Long-term investment securities ...288... -
Page 60
... OF INCOME For the year ended December 31, 2002 2001 2000 (in thousands, except per share results) Revenues: Premiums ...$10,930,397 Administrative services fees ...244,396 Investment and other income ...86,388 Total revenues ...Operating expenses: Medical ...Selling, general and administrative... -
Page 61
...' EQUITY Common Stock Issued Shares Amount Capital In Excess of Par Value Accumulated Unearned Other Restricted Retained Comprehensive Stock Treasury Earnings Income (Loss) Compensation Stock $(28,490) - $ (1,510) - $ - - Total Stockholders' Equity $1,268,011 90,052 Balances, January 1, 2000... -
Page 62
... the year ended December 31, 2002 2001 2000 (in thousands) Cash flows from operating activities Net income ...Adjustments to reconcile net income to net cash provided by operating activities: Non-cash restructuring charge ...Depreciation and amortization ...Amortization of restricted stock ...Loss... -
Page 63
...Under one federal government contract with the Centers for Medicare and Medicaid Services, or CMS, we provide health insurance coverage for Medicare+Choice members in Florida, accounting for approximately 16% of our total premiums and administrative services fees in 2002. We manage our business with... -
Page 64
...Medicaid programs are generally multi-year contracts subject to annual renewal provisions. Our Medicare+Choice contracts with the federal government renew annually. We bill and collect premium and administrative fee remittances from employer groups and some individual Medicare+Choice members monthly... -
Page 65
.... Administrative services fees cover the processing of claims, offering access to our provider networks and clinical programs, and responding to customer service inquiries from members of self-funded employers. Under ASO contracts, selffunded employers and, for TRICARE ASO, the Department of Defense... -
Page 66
...incurred to provide health insurance coverage to members, as well as estimates of future payments to hospitals and others for medical care provided prior to the balance sheet date. Capitation payments represent monthly contractual fees disbursed to primary care physicians and other providers who are... -
Page 67
... operating our company such as professional and general liability, employee workers' compensation, and officer and director errors and omissions risks. Professional and general liability risks may include, for example, medical malpractice claims and disputes with members regarding benefit coverage... -
Page 68
..., to our fixed-based stock option awards. For the years ended 2002 2001 2000 (in thousands, except per share results) Net income, as reported ...Add: Restricted stock compensation expense included in reported net income, net of related tax ...Deduct: Total stock-based employee compensation expense... -
Page 69
... additional disclosure in filings issued after January 31, 2003. The adoption of FIN 46 is not expected to have a material impact on our financial position, results of operations or cash flows. In January 2003, the FASB issued Statement No. 148, Accounting for Stock-Based Compensation- Transition... -
Page 70
... for sale at December 31, 2002, regardless of their balance sheet classification, are shown below. Expected maturities may differ from... participation in a securities lending program where we loan certain investment securities for short periods of time in exchange for collateral, consisting of cash or... -
Page 71
...: For the years ended 2002 2001 2000 (in thousands, except per share results) Net income: Reported net income ...Add back: goodwill amortization expense, net of tax ...Adjusted net income ...Basic earnings per common share: Reported basic earnings per common share ...Add back: goodwill amortization... -
Page 72
... resulted from claims being settled for amounts less than originally estimated. 6. INCOME TAXES The provision for income taxes consisted of the following: For the year ended December 31, 2002 2001 2000 (in thousands) Current provision (benefit): Federal ...States and Puerto Rico ...Total current... -
Page 73
... was different from the amount computed using the federal statutory rate due to the following: For the year ended December 31, 2002 2001 2000 (in thousands) Income tax provision at federal statutory rate ...$ 73,477 $ 64,078 $ 39,897 States and Puerto Rico income taxes, net of federal benefit ...10... -
Page 74
... and profitability, we have concluded that future operating income and capital gains will be sufficient to give rise to tax expense and capital gains to recover all deferred tax assets, net of the valuation allowance. 7. DEBT The following table presents our short-term and long-term debt outstanding... -
Page 75
... compliance assuming the more restrictive future financial covenant requirements were applicable at December 31, 2002. Commercial Paper Programs We maintain indirect access to the commercial paper market through our conduit commercial paper financing program. Under this program, a third party issues... -
Page 76
... of the years ended December 31, 2002, 2001 and 2000 were attributable to favorable loss development, primarily related to medical malpractice exposures. Beginning January 1, 2002, we reduced the amount of coverage purchased from third party insurance carriers, causing an increase in the net reserve... -
Page 77
... from insurance ...Total net reserve ...9. EMPLOYEE BENEFIT PLANS Employee Savings Plan $ 53,461 209,302 262,763 34,290 108,305 142,595 $120,168 $ 60,087 241,431 301,518 42,322 144,651 186,973 $114,545 We have defined contribution retirement and savings plans covering eligible employees. Our... -
Page 78
...of $14.09. We account for our stock option plan under APB No. 25 and accordingly no employee compensation cost has been recognized for our fixed-based stock option awards other than for modifications of option terms that result in a new measurement date. Compensation expense related to modifications... -
Page 79
...of Series A Participating Preferred Stock at a price of $145 per share. This plan expires in 2006. Regulatory Requirements Certain of our subsidiaries operate in states that regulate the payment of dividends, loans or other cash transfers to Humana Inc., our parent company, require minimum levels of... -
Page 80
... number of years. If RBC were fully implemented by all states at December 31, 2002, each of our subsidiaries would be in compliance, and we would have $358.8 million of aggregate capital and surplus above the minimum level required under RBC. One TRICARE subsidiary under the Regions 3 and 4 contract... -
Page 81
... represents 86% of our total Medicaid membership as of December 31, 2002. The term of each of these contracts is three years, subject to annual renewal options with the Health Insurance Administration in Puerto Rico. Our Medicaid contracts in Florida and Illinois generally are annual contracts. 75 -
Page 82
...on our financial position, results of operations and cash flows. Legal Proceeding Securities Litigation In late 1997, three purported class action complaints were filed in the United States District Court for the Southern District of Florida by former stockholders of Physician Corporation of America... -
Page 83
...subclass consists of medical doctors who provided services to any person insured in California by any defendant when the doctor was not bound to arbitrate the claim. On October 10, 2002, the defendants asked the Court of Appeals for the Eleventh Circuit to review the class certification decision. On... -
Page 84
... we entered into a five-year Corporate Integrity Agreement, or CIA, with the Office of Inspector General, or OIG, of the Department of Health and Human Services. Under the CIA, we are obligated to, among other things, provide training, conduct periodic audits and make periodic reports to the OIG. In... -
Page 85
... financial position, results of operations and cash flows. 13. ACQUISITIONS AND DIVESTITURES Acquisitions On May 31, 2001, we acquired the outstanding shares of common stock of a newly-formed Anthem Health Insurance Company subsidiary responsible for administering TRICARE benefits in Regions 2 and... -
Page 86
... including customer service, claim administration, clinical operations, provider network administration, as well as other corporate and fieldbased positions. As part of the plan, we expect to hire approximately 300 employees to support newly consolidated operations, thereby resulting in a net... -
Page 87
... operations. 15. SEGMENT INFORMATION We manage our business with two segments: Commercial and Government. The Commercial segment consists of members enrolled in products marketed to employer groups and individuals, and includes three lines of business: fully insured medical, administrative services... -
Page 88
... For the year ended December 31, 2002 2001 2000 (in thousands) Revenues: Premiums: Fully insured: HMO ...PPO ...Total fully insured ...Specialty ...Total premiums ...Administrative services fees ...Investment and other income ...Total revenues ...Operating expenses: Medical ...Selling, general and... -
Page 89
...the year ended December 31, 2002 2001 2000 (in thousands) Revenues: Premiums: Medicare+Choice ...$2,629,597 TRICARE ...2,001,474 Medicaid ...462,998 Total premiums ...Administrative services fees ...Investment and other income ...Total revenues ...Operating expenses: Medical ...Selling, general and... -
Page 90
... financial position of Humana Inc. and its subsidiaries at December 31, 2002 and 2001, and the results oftheir operations and their cash flows for each of the three years in the period ended December 31, 2002, in conformity with accounting principles generally accepted in the United States of... -
Page 91
... unaudited results of operations for the years ended December 31, 2002, and 2001 follows: First For the year ended December 31, 2002 Second Third Fourth (a) (in thousands, except per share results) Total revenues ...Income (loss) before income taxes ...Net income (loss) ...Basic earnings (loss) per... -
Page 92
... Vice President-Chief Service and Information Officer Senior Vice President-Chief Human Resources Officer Senior Vice President-General Counsel Senior Vice President-Strategy and Corporate Development Senior Vice President-Chief Innovation Officer Senior Vice President-Chief Marketing Officer Senior... -
Page 93
... Insurance Company in Roseland, New Jersey. Ms. Hathcock currently serves as Senior Vice President and Chief Human Resources Officer having held this position since May 1999. Prior to joining the Company, Ms. Hathcock served as Vice President of Human Resources & Development for US Airways Group... -
Page 94
... Within 90 days prior to the filing date of this report, we carried out an evaluation, under the supervision and with the participation of our Chief Executive Officer, or CEO and Chief Financial Officer, or CFO, of the effectiveness of the design and operation of our disclosure controls and... -
Page 95
...the Company's Proxy Statement covering the Annual Meeting of Stockholders held on February 18, 1993, is incorporated by reference herein. Amendment No. 2 to the 1989 Stock Option Plan for Employees. Exhibit 10(e) to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 1993... -
Page 96
... providing for termination benefits in the event of a change of control. Exhibit 10(m) to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 1997, is incorporated by reference herein. Humana Inc. 2002 Management Incentive Compensation Plan ("MIP") description, filed... -
Page 97
... herein. Humana Supplemental Executive Retirement Plan, as amended. Exhibit 10(t) to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 1994, is incorporated by reference herein. Letter agreement with Company officers concerning health insurance availability. Exhibit... -
Page 98
HUMANA INC. SCHEDULE I-PARENT COMPANY FINANCIAL INFORMATION CONDENSED BALANCE SHEETS December 31, 2002 2001 (in thousands, except share amounts) ASSETS Current assets: Cash and cash equivalents ...Other current assets ...Total current assets ...Property and equipment, net ...Investments in ... -
Page 99
... INFORMATION CONDENSED STATEMENTS OF OPERATIONS For the year ended December 31, 2002 2001 2000 (in thousands) Revenues: Management fees charged to operating subsidiaries ...Investment (loss) income and other income, net ...Expenses: Selling, general and administrative ...Depreciation ...Interest... -
Page 100
... For the year ended December 31, 2002 2001 2000 (in thousands) Net cash provided by operating activities ...Cash flows from investing activities: Acquisitions ...Purchases of investment securities ...Proceeds from sale of investment securities ...Purchases of property and equipment, net ...Capital... -
Page 101
... fee for reimbursement of certain centralized services provided to its subsidiaries including information systems, disbursement, investment and cash administration, marketing, legal, finance, and medical and executive management oversight. Guarantee Through indemnity agreements approved by state... -
Page 102
..., thereto duly authorized. HUMANA INC. By: /s/ JAMES H. BLOEM James H. Bloem Senior Vice President and Chief Financial Officer Date: March 21, 2003 Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the... -
Page 103
... I, Michael B. McCallister, principal executive officer of Humana Inc., certify that: 1. 2. I have reviewed this annual report on Form 10-K of Humana Inc.; Based on my knowledge, this annual report does not contain any untrue statement of a material fact or omit to state a material fact necessary to... -
Page 104
... I, James H. Bloem, principal financial officer of Humana Inc., certify that: 1. 2. I have reviewed this annual report on Form 10-K of Humana Inc.; Based on my knowledge, this annual report does not contain any untrue statement of a material fact or omit to state a material fact necessary to make... -
Page 105
-
Page 106
-
Page 107
.... Michael B. McCallister President and Chief Executive Officer - Humana Inc. W. Ann Reynolds, Ph.D. Director - Center for Community Outreach Development - The University of Alabama at Birmingham Corporate Headquarters The Humana Building 500 West Main Street Louisville, Kentucky 40202 (502) 580-1000... -
Page 108
GN-32072-HH