Humana 2002 Annual Report Download - page 11
Download and view the complete annual report
Please find page 11 of the 2002 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.HMO
Our health maintenance organization, or HMO, products provide prepaid health insurance coverage to our
members through a network of independent primary care physicians, specialty physicians and other health care
providers who contract with the HMO to furnish such services. Primary care physicians generally include
internists, family practitioners and pediatricians. Generally, the member’s primary care physician must approve
access to certain specialty physicians and other health care providers. These other health care providers include,
among others, hospitals, nursing homes, home health agencies, pharmacies, mental health and substance abuse
centers, diagnostic centers, optometrists, outpatient surgery centers, dentists, urgent care centers and durable
medical equipment suppliers. Because the primary care physician must generally approve access to many of
these other health care providers, the HMO product is the most restrictive form of managed care.
An HMO member, typically through the member’s employer, pays a monthly fee, which generally covers,
with some copayments, health care services received from or approved by the member’s primary care physician.
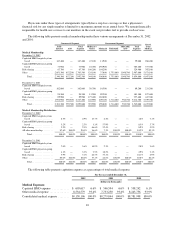
For the year ended December 31, 2002, commercial HMO premium revenues totaled approximately $2.6 billion,
or 23.4% of our total premiums and ASO fees.
PPO
Our preferred provider organization, or PPO, products include some elements of managed health care;
however, they typically include more cost-sharing with the member, through copayments and annual deductibles.
PPOs are also similar to traditional health insurance because they provide a member with more freedom to
choose a physician or other health care provider. In a PPO, the member is encouraged, through financial
incentives, to use participating health care providers, which have contracted with the PPO to provide services at
favorable rates. In the event a member chooses not to use a participating health care provider, the member may
be required to pay a greater portion of the provider’s fees. For the year ended December 31, 2002, commercial
PPO premium revenues totaled approximately $2.9 billion, or 25.8% of our total premiums and ASO fees.
Individual Products
In June 2002, we introduced HumanaOne, our first product marketed directly to individuals. We have
introduced this product in select markets where we can utilize our existing networks and distribution channels.
Administrative Services Only
We offer an administrative services only, or ASO, product to those who self-insure their employee health
plans. We receive fees to provide administrative services which generally include the processing of claims,
offering access to our provider networks and clinical programs, and responding to customer services inquiries
from members of self-funded employers. These products may include all of the same benefit and product design
characteristics of our fully insured PPO and HMO products described above, however, under ASO contracts,
self-funded employers retain the risk of financing the cost of health benefits. For the year ended December 31,
2002, commercial administrative services fees totaled $103.2 million, or 0.9% of our total premiums and ASO
fees.
Specialty Products
We also offer various specialty products including dental, group life and short-term disability. At
December 31, 2002, we had approximately 1.6 million specialty members. For the year ended December 31,
2002, specialty product premium revenues were approximately $337.3 million, or 3.1% of our total premiums
and ASO fees.
5