Humana 2002 Annual Report Download - page 13
Download and view the complete annual report
Please find page 13 of the 2002 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.On May 31, 2001, we acquired for $43.5 million the outstanding shares of common stock of a newly formed
Anthem Alliance Health Insurance Company subsidiary responsible for administering TRICARE benefits for
Regions 2 and 5 to approximately 1.2 million eligible members in Illinois, Indiana, Kentucky, Michigan, a
portion of Missouri, North Carolina, Ohio, Tennessee, Virginia, Wisconsin and West Virginia.
We currently are in negotiations with the Department of Defense to extend our TRICARE contracts that
expire on April 30, 2003 for Regions 2 and 5 and June 30, 2003 for Regions 3 and 4. We believe we will be able
to successfully extend our TRICARE contracts under substantially the same terms for one additional year plus a
one year renewal option which should continue our contracts through the new TRICARE Next Generation, or
T-Nex, transition described below. Historical pretax profit margins for our TRICARE business have generally
ranged from 2 to 4 percent. We expect margins to continue in this range during 2003.
The Department of Defense recently announced a plan to consolidate the total number of prime contracts
from seven to three under the new T-Nex program. The Department of Defense has stated that a bidder can be
awarded only one prime contract, although a bidder would be allowed to secondarily participate in another
contract. We submitted a bid in January 2003 to participate as a prime contractor for the South region.
Additionally, we partnered with Aetna Government Health Plans, LLC, a subsidiary of Aetna, Inc. to participate
as a subcontractor should Aetna Government Health Plans, LLC be awarded the North region. An announcement
of the awards is expected in mid to late 2003 with transition to the new regions not expected until mid to late
2004. At this time we are unable to predict whether we will be awarded a contract, or the effective date of the
contract.
If we are a successful bidder on the South region, we do not expect a material change to our consolidated
financial position, results of operations, or cash flows, although TRICARE profits could decline slightly.
TRICARE membership would not materially change from current levels. TRICARE revenues and expenses
would decline by approximately 20% as a result of certain benefits, e.g. pharmacy, which are included under our
current contract, being excluded and under separate T-Nex contracts in the future.
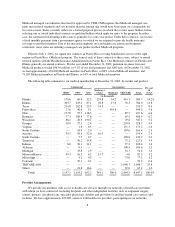
Currently, three health benefit options are available to TRICARE beneficiaries. In addition to a traditional
indemnity option, participants may enroll in an HMO-like plan with a point-of-service option or take advantage
of reduced copayments by using a network of preferred providers. We have subcontracted with third parties to
provide various administration and specialty services under the contracts. For the year ended December 31, 2002,
TRICARE premium revenues were approximately $2.0 billion, or 17.9% of our total premiums and ASO fees.
At December 31, 2002, we had 1,048,700 TRICARE ASO members for which the Department of Defense
retains the risk of financing the cost of their health benefits. We obtained these members from our acquisition of
Regions 2 and 5, and from two government programs that allow senior members to continue in the TRICARE
program even after becoming Medicare eligible, which is normally age 65. The first of these programs, called
TRICARE Senior Pharmacy, became effective April 1, 2001. Under this government administrative services
program, senior TRICARE members receive certain pharmacy benefits not covered under Medicare. On
October 1, 2001, the TRICARE For Life program became effective, and expanded coverage to include medical
benefits as well. We are engaged by the Department of Defense to provide these administrative services through
change orders to our existing TRICARE contracts. Once T-Nex becomes effective, our participation in these
ASO programs will allow us to competitively bid for certain of the services under separate contracts. Although
we will not bid on the TRICARE for Life contract under T-Nex, we may bid on other services under separate T-
Nex contracts. Anticipated changes to these benefits contracted separately contribute to the expected 20% decline
in total TRICARE revenue discussed above. For the year ended December 31, 2002, TRICARE administrative
services fees totaled $141.2 million, or 1.3% of our total premiums and ASO fees.
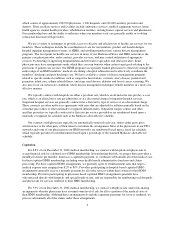
Medicaid Product
Medicaid is a federal program that is state-operated to facilitate the delivery of health care services to low-
income residents. Each state that chooses to do so develops, through a state specific regulatory agency, a
7