Humana 2002 Annual Report Download - page 3
Download and view the complete annual report
Please find page 3 of the 2002 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.plans that ranged from traditional HMO and PPO offerings to CoverageFirst, a bold, new, consumer-driven
approach. In addition, we developed groundbreaking online educational tools to make SmartSuite easy to choose
and use, including a PlanWizard during the selection process, a personalized home page and fast access to Web-
based customer service.
CoverageFirst features reduced premiums for consumers. It offers a basic layer of first-dollar coverage,
$500 per member, supplied by the employer through the plan. The next layer is either a $1,000 or $2,500
deductible for which the employee is responsible, with a final layer of comprehensive PPO coverage.
An online PlanWizard tool helps employees select the plan that’s right for them. Throughout the plan year,
guidance in the form of e-mail alerts (in which we notify members who have had prescriptions filled of the
existence of comparable lower-cost options), voice-activated-technology health reminders and Web-based
customer service give consumers the power to take control of their health and health spending.
For Humana and our employees, the result has been win-win. With a full year of claims experience, our
anticipated 19.2 percent cost increase for Louisville associates resulted in a rise of only 4.9 percent – saving the
company $2.1 million. The 4,800 employees and their dependents actually paid less as a percentage of total costs
(19 percent vs. 21 percent) than they did the year before. In the same vein, Trover Solutions, our initial external
client, finished its first SmartSuite year having paid less in total employee claims than it did the year before. We
have now rolled out SmartSuite to all our markets.
Encouraged by these results, we’re continuing to innovate. Our “next-generation” product series,
SmartSelect, preserves the consumer-centric features of SmartSuite and also gives employees the ability, through
Web-based tools, to customize health benefits for themselves and their families, based on individual health
histories and anticipated spending in the upcoming plan year.
2002 Milestones
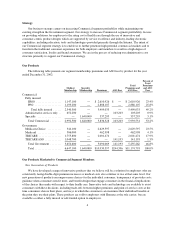
With a new product suite as well as strong showings from our traditional product offerings, our Commercial
segment improved substantially in 2002. Medical membership grew 3.4 percent – the product of increased
proposal activity as well as a targeted approach to prospects most likely to buy from us.
Not only has the SmartSuite product grown appreciably since its launch in the second quarter of 2002, it has
also generated significant excitement among employers, brokers and consultants. Our sales force is “cross-
benefiting” from the opportunity to present our traditional products to SmartSuite prospects, and vice versa. In
addition, our small group segment began growing again in the second half of 2002.
HumanaOne, our first product designed for the individual market, was also launched this year. Individuals
are responding positively to HumanaOne’s benefit design and the access it gives to our broad-based provider
networks. In addition, our electronically enabled customer support services are well-suited to the self-service
focus of HumanaOne.
Toward the end of 2002 we announced plans to streamline service operations by consolidating our current
seven service center locations to four and by reducing our workforce by 2,300, or 17 percent. These moves signal
a new era of productivity for Humana. While membership has grown, service metrics have appreciably
improved, demonstrating our growing ability to “do more with less.”
Within service operations we reached a milestone in April when, for the first time, more than half of all
customer contacts on our largest claims-paying platform were handled electronically, rather than through a
customer service representative on the phone. Our rate of claims adjudicated electronically is nearing 75 percent.
And our claims inventory process speed is exceptional – making us the partner of choice for many providers,
employers and consumers who are delighted with the hassle-free service they receive when claims are paid
quickly. Our unprocessed claims inventories on hand are now down to 4 days versus 5 days at Dec. 31, 2001 and
11 days at the end of 2000.