Humana 2008 Annual Report Download - page 107
Download and view the complete annual report
Please find page 107 of the 2008 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Humana Inc.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
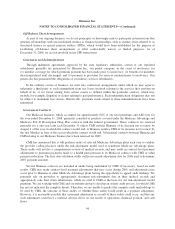
(“ERISA”) (the “Amended ERISA Complaint”), which alleges, among other things, that the ERISA Defendants
breached their fiduciary duties under ERISA by (i) offering Humana stock as an investment option within the
Plans and making contributions in Humana stock when that stock was not a prudent investment for participants’
retirement savings, (ii) providing misleading information, knowingly concealing information, and failing to
provide participants with complete and accurate information regarding Humana’s financial condition, its internal
controls, its business practices, and the prudence of investing in its stock, (iii) failing to adequately monitor the
Plans’ fiduciaries and remove any fiduciaries whose performance was inadequate, and (iv) failing to avoid
conflicts of interest and to serve the interests of the Plans’ participants and beneficiaries with undivided loyalty.
The Amended ERISA Complaint also alleges that certain defendants are liable for those breaches as
co-fiduciaries because they enabled, knowingly participated in and/or knew of and failed to remedy those
breaches. The Amended ERISA Complaint seeks the following relief, among other things: (i) repayment of
alleged losses to the Plans, restoration of profits that the ERISA Defendants allegedly made using the Plans’
assets, and restoration of Plan participants’ lost profits; (ii) imposition of a constructive trust on any amounts by
which the ERISA Defendants were unjustly enriched at the expense of the Plans; (iii) appointment of one or
more independent fiduciaries to participate in managing the Plans’ investment in Humana stock; (iv) actual
damages; (v) an award of plaintiffs’ legal fees and costs; and (vi) equitable restitution and other equitable
monetary relief. On December 8, 2008, the ERISA Defendants filed a motion seeking dismissal of the case. The
plaintiffs filed their opposition to that motion on January 29, 2009. The ERISA Defendants’ reply brief in support
of their motion is due on March 2, 2009.
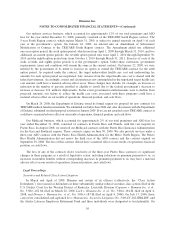
Provider Litigation
Humana Military Healthcare Services, Inc. (“HMHS”) has been named as a defendant in Sacred Heart
Health System, Inc., et al. v. Humana Military Healthcare Services Inc., Case No. 3:07-cv-00062 MCR/EMT (the
“Sacred Heart” Complaint), a class action lawsuit filed on February 5, 2007 in the U.S. District Court for the
Northern District of Florida asserting contract and fraud claims against HMHS. The Sacred Heart Complaint
alleges, among other things, that, HMHS breached its network agreements with a class of hospitals, including the
seven named plaintiffs, in six states that contracted for reimbursement of outpatient services provided to
beneficiaries of the Department of Defense’s TRICARE health benefits program (“TRICARE”). The Complaint
alleges that HMHS breached its network agreements when it failed to reimburse the hospitals based on
negotiated discounts for non-surgical outpatient services performed on or after October 1, 1999, and instead
reimbursed them based on published CHAMPUS Maximum Allowable Charges (so-called “CMAC rates”).
HMHS denies that it breached the network agreements with the hospitals and asserted a number of defenses to
these claims. The Complaint seeks, among other things, the following relief for the purported class members:
(i) damages as a result of the alleged breach of contract by HMHS, (ii) taxable costs of the litigation,
(iii) attorneys fees, and (iv) any other relief the court deems just and proper. Separate and apart from the class
relief, named plaintiff Sacred Heart Health System Inc. requests damages and other relief the court deems just
and proper for its individual claim against HMHS for fraud in the inducement to contract. On September 25,
2008, the district court certified a class consisting of “all institutional healthcare service providers in TRICARE
former Regions 3 and 4 which had network agreements with [HMHS] to provide outpatient non-surgical services
to CHAMPUS/TRICARE beneficiaries as of November 18, 1999, excluding those network providers who
contractually agreed with [HMHS] to submit any such disputes with [HMHS] to arbitration.” HMHS is
challenging the certification of this class action. On October 9, 2008, HMHS petitioned the U.S. Court of
Appeals for the Eleventh Circuit pursuant to Federal Rule of Civil Procedure 23(f) for permission to appeal on an
interlocutory basis. On November 14, 2008, the Court of Appeals granted HMHS’s petition. On November 21,
2008, the district court stayed proceedings in the case pending the result of the appeal on the class issue or until
further notice.
Humana intends to defend each of these actions vigorously.
97