Humana 2008 Annual Report Download - page 108
Download and view the complete annual report
Please find page 108 of the 2008 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Humana Inc.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Other Lawsuits and Regulatory Matters
Our current and past business practices are subject to review by various state insurance and health care
regulatory authorities and other state and federal regulatory authorities. These authorities regularly scrutinize the
business practices of health insurance and benefits companies. These reviews focus on numerous facets of our
business, including claims payment practices, competitive practices, commission payments, privacy issues,
utilization management practices, and sales practices. Some of these reviews have historically resulted in fines
imposed on us and some have required changes to some of our practices. We continue to be subject to these
reviews, which could result in additional fines or other sanctions being imposed on us or additional changes in
some of our practices.
In February 2008, the New York Attorney General initiated an industry-wide investigation into certain
provider-payment practices. Like other companies, we received subpoenas in connection with this matter. We
have cooperated fully with the investigation. Our operations in New York consist primarily of Medicare business
which is not subject to the investigation. Subsequently, the New York Attorney General has settled this matter
with certain other industry participants. In addition, we have also responded to similar requests for information
from other states’ attorneys general.
We also are involved in various other lawsuits that arise, for the most part, in the ordinary course of our
business operations, including employment litigation, claims of medical malpractice, bad faith, nonacceptance or
termination of providers, anticompetitive practices, improper rate setting, failure to disclose network discounts
and various other provider arrangements, intellectual property matters, and challenges to subrogation practices.
We also are subject to claims relating to performance of contractual obligations to providers, members, and
others, including failure to properly pay claims, challenges to our implementation of the new Medicare
prescription drug program and other litigation.
Personal injury claims and claims for extracontractual damages arising from medical benefit denials are
covered by insurance from our wholly owned captive insurance subsidiary and excess carriers, except to the
extent that claimants seek punitive damages, which may not be covered by insurance in certain states in which
insurance coverage for punitive damages is not permitted. In addition, insurance coverage for all or certain forms
of liability has become increasingly costly and may become unavailable or prohibitively expensive in the future.
The outcome of the securities litigation, provider litigation, and other current or future suits or governmental
investigations cannot be accurately predicted with certainty, and it is reasonably possible that their outcomes
could have a material adverse effect on our results of operations, financial position, and cash flows.
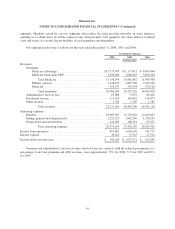
17. SEGMENT INFORMATION
We manage our business with two segments: Government and Commercial. The Government segment
consists of beneficiaries of government benefit programs, and includes three lines of business: Medicare,
Military, and Medicaid. The Commercial segment consists of members enrolled in our medical and specialty
products marketed to employer groups and individuals. We identified our segments in accordance with the
aggregation provisions of SFAS 131,which aggregates products with similar economic characteristics. These
characteristics include the nature of customer groups as well as pricing, benefits, and underwriting requirements.
These segment groupings are consistent with information used by our Chief Executive Officer.
The accounting policies of each segment are the same and are described in Note 2. The results of each
segment are measured by income before income taxes. We allocate all selling, general and administrative
expenses, investment and other revenue, interest expense, and goodwill, but no other assets or liabilities, to our
98