Humana 2008 Annual Report Download - page 45
Download and view the complete annual report
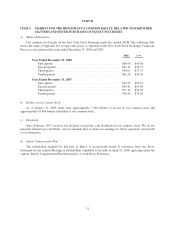
Please find page 45 of the 2008 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.We offer three Medicare stand-alone prescription drug plans, or PDPs, under the Medicare Part D program:
our Standard, Enhanced, and Complete products. These plans provide varying degrees of coverage. In order to
offer these plans in a given year, in June of the preceding year we must submit bids to CMS for approval. During
2008, we experienced prescription drug claim expenses for our Medicare stand-alone PDPs that were higher than
we had originally assumed in the bid that we submitted to CMS in June 2007. These higher claim levels for our
Medicare stand-alone PDPs reflected a combination of several variances between our actuarial bid assumptions
versus our experience. These variances resulted from, among other things, differences between the actuarial
utilization assumptions (which are our attempts to predict members’ future utilization of drugs) in the bids for
our Enhanced plans versus our actual claims experience in 2008, as well as an increase in the percentage of
higher cost members in both our Standard and Enhanced plans. The lower stand-alone PDP operating results
primarily caused the decrease in consolidated earnings during 2008 compared to 2007. We believe we have
addressed these issues for 2009, based on enhancements made to our bid development and review processes. In
January 2009, stand-alone PDP membership declined by 924,000 members to approximately 2,143,000, resulting
primarily from our competitive positioning as we realigned stand-alone PDP premium and benefit structures to
correspond with our pharmacy claims experience.
The enactment of the Medicare Improvements for Patients and Providers Act of 2008, or the Act, in July
2008 could affect our Medicare operations. Principally, beginning in 2011 sponsors of Medicare Advantage
PFFS plans will be required to contract with providers to establish adequate networks, except in geographic areas
that CMS determines have fewer than two network-based Medicare Advantage plans. Nearly 60% of our
Medicare Advantage members are already enrolled in one of our network-based plans as of January 31, 2009. We
are implementing various operational and strategic initiatives that are intended to answer the challenges
presented by the Act. In addition, approximately 80% of our PFFS enrollees at January 1, 2009 reside in
geographies where we have developed a PPO network and offer a PPO plan. We will continue to develop our
PPO network and build network-based plan offerings to address the network restriction. Nonetheless, there can
be no assurance that we will be able to successfully implement those initiatives. Failure to implement this
strategy may result in a material adverse effect on our results of operations, financial position, and cash flows.
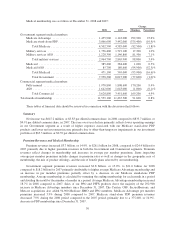
Our quarterly Government segment earnings and operating cash flows are particularly impacted by the
Medicare Part D benefit design and changes in the composition of our membership. The Medicare Part D benefit
design results in coverage that varies as a member’s cumulative out-of-pocket costs pass through successive
stages of a member’s plan period which begins January 1 for renewals. These plan designs generally result in us
sharing a greater portion of the responsibility for total pharmacy costs in the early stages and less in the latter
stages. As a result the Government segment’s benefit ratio generally improves as the year progresses. In addition,
the number of low-income senior members as well as year-over-year changes in the mix of membership in our
stand-alone PDP products, Standard, Enhanced, and Complete, affect the quarterly benefit ratio pattern.
Commercial Segment
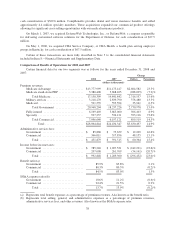
We continue to increase the diversification of our Commercial segment membership. Commercial segment
medical membership increased 169,200 members, or 4.9% from December 31, 2007 to 3,620,800 members at
December 31, 2008, primarily as a result of the acquisitions of Cariten and OSF discussed more fully below,
which together added approximately 83,100 fully-insured members and 51,300 ASO members. The remaining
increase primarily was due to enrollment gains in strategic areas of commercial growth. Individual membership
increased 32%, Smart plans and other consumer offerings membership grew 19%, and small group membership
was up 1% at December 31, 2008 compared to December 31, 2007.
In addition, our Commercial segment revenues grew in 2008 through expanded and new specialty product
offerings with the acquisitions of CompBenefits and KMG in the fourth quarter of 2007. These acquisitions
significantly increased our dental membership and added new product offerings, including vision and other
voluntary employee benefits including supplemental health products such as cancer, critical illness, and accident
policies. Along with our 2005 acquisition of Corphealth, Inc. (d/b/a LifeSynch), a behavioral health care
35