Humana 2008 Annual Report Download - page 68
Download and view the complete annual report
Please find page 68 of the 2008 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.associated with a closed block of long-term care policies acquired in connection with the November 30, 2007
KMG acquisition. Long-term care policies provide for long-duration coverage and, therefore, our actual claims
experience will emerge many years after assumptions have been established. The risk of a deviation of the actual
morbidity and mortality rates from those assumed in our reserves are particularly significant to our closed block
of long-term care policies. We monitor the loss experience of these long-term care policies and, when necessary,
apply for premium rate increases through a regulatory filing and approval process in the jurisdictions in which
such products were sold. We expect to file premium rate increases in 2009. To the extent premium rate increases
or loss experience vary from our acquisition date assumptions, future adjustments to reserves could be required.
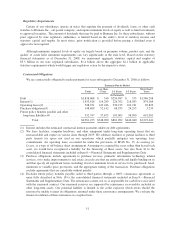
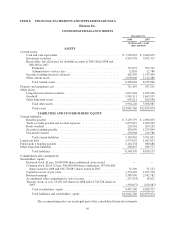
In addition, future policy benefits payable include amounts of $232.0 million at December 31, 2008 and $239.7
million at December 31, 2007 which are subject to 100% coinsurance agreements as more fully described in Note
18 to the consolidated financial statements included in Item 8.—Financial Statements and Supplementary Data,
and as such are offset by a related reinsurance recoverable included in other long-term assets.
As previously discussed, our reserving practice is to consistently recognize the actuarial best estimate of our
ultimate liability for claims. Actuarial standards require the use of assumptions based on moderately adverse
experience, which generally results in favorable reserve development, or reserves that are considered redundant.
An increase in the absolute dollar amount of redundancy over the last three years primarily has resulted from the
growth in our Medicare business, coupled with the application of consistent reserving practices. When we
recognize a release of the redundancy, we disclose the amount that is not in the ordinary course of business, if
material. We believe we have consistently applied our methodology in determining our best estimate for benefits
payable.
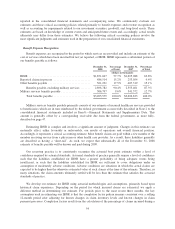
Revenue Recognition
We generally establish one-year commercial membership contracts with employer groups, subject to
cancellation by the employer group on 30-day written notice. Our Medicare contracts with CMS renew annually.
Our military services contracts with the federal government and our contracts with various state Medicaid
programs generally are multi-year contracts subject to annual renewal provisions.
Our commercial contracts establish rates on a per member basis for each month of coverage. Our Medicare
and Medicaid contracts also establish monthly rates per member. However, our Medicare contracts also have
additional provisions as outlined in the following separate section.
Premium revenues and ASO fees are estimated by multiplying the membership covered under the various
contracts by the contractual rates. In addition, we adjust revenues for estimated changes in an employer’s
enrollment and individuals that ultimately may fail to pay. Enrollment changes not yet reported by an employer
group, an individual, or the government, also known as retroactive membership adjustments, are estimated based
on available data and historical trends. We routinely monitor the collectibility of specific accounts, the aging of
receivables, historical retroactivity trends, as well as prevailing and anticipated economic conditions, and reflect
any required adjustments in the current period’s revenue.
We bill and collect premium and administrative fee remittances from employer groups and members in our
Medicare and individual products monthly. We receive monthly premiums and administrative fees from the
federal government and various states according to government specified reimbursement rates and various
contractual terms. Changes in revenues from CMS for our Medicare products resulting from the periodic changes
in risk-adjustment scores for our membership are recognized when the amounts become determinable and the
collectibility is reasonably assured.
Medicare Part D Provisions
On January 1, 2006, we began covering prescription drug benefits in accordance with Medicare Part D
under multiple contracts with CMS. The payments we receive monthly from CMS and members, which are
determined from our annual bid, represent amounts for providing prescription drug insurance coverage. We
recognize premium revenues for providing this insurance coverage ratably over the term of our annual contract.
58