Humana 2008 Annual Report Download - page 69
Download and view the complete annual report
Please find page 69 of the 2008 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Our CMS payment is subject to risk sharing through the Medicare Part D risk corridor provisions. In addition, we
receive and disburse amounts for portions of prescription drug costs for which we are not at risk, as described
more fully below.
The risk corridor provisions compare costs targeted in our bids to actual prescription drug costs, limited to
actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding
certain thresholds may result in CMS making additional payments to us or require us to refund to CMS a portion
of the premiums we received. We estimate and recognize an adjustment to premium revenues related to these risk
corridor provisions based upon pharmacy claims experience to date as if the annual contract were to terminate at
the end of the reporting period. Accordingly, this estimate provides no consideration to future pharmacy claims
experience. We record a receivable or payable at the contract level and classify the amount as current or long-
term in the consolidated balance sheets based on the expected settlement.
The estimate of the settlement associated with risk corridor provisions requires us to consider factors that
may not be certain, including, among others, member eligibility differences with CMS. In 2008, we paid $78.7
million related to our reconciliation with CMS regarding the 2007 Medicare Part D risk corridor provisions
compared to our estimate of $102.6 million at December 31, 2007. In 2007, we paid $725.5 million related to our
reconciliation with CMS regarding the 2006 Medicare Part D risk corridor provisions compared to our estimate
of $738.7 million at December 31, 2006. 2006 marked the first year of providing for the risk corridor estimate
and required us to consider factors which were not certain, including certain first year implementation issues. The
net asset associated with the 2008 risk corridor estimate, which will be settled in 2009, was $55.4 million at
December 31, 2008.
Reinsurance and low-income cost subsidies represent reimbursements from CMS in connection with the
Medicare Part D program for which we assume no risk. Reinsurance subsidies represent reimbursements for
CMS’s portion of prescription drug costs which exceed the member’s out-of-pocket threshold, or the catastrophic
coverage level. Low-income cost subsidies represent reimbursements from CMS for all or a portion of the
deductible, the coinsurance and co-payment amounts above the out-of-pocket threshold for low-income
beneficiaries. Monthly prospective payments from CMS for reinsurance and low-income cost subsidies are based
on assumptions submitted with our annual bid. A reconciliation and related settlement of CMS’s prospective
subsidies against actual prescription drug costs we paid is made after the end of the year. We account for these
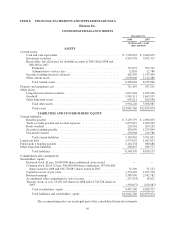
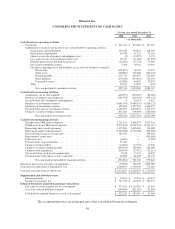
subsidies as a deposit in our consolidated balance sheets and as a financing activity in our consolidated
statements of cash flows. We do not recognize premium revenues or benefit expense for these subsidies. Receipt
and payment activity is accumulated at the contract level and recorded in our consolidated balance sheets in other
current assets or trade accounts payable and accrued expenses depending on the contract balance at the end of the
reporting period. Gross financing receipts were $2,761.3 million and gross financing withdrawals were $2,572.6
million during 2008. CMS subsidy activity recorded to the consolidated balance sheets at December 31, 2008
was $322.1 million to other current assets and $219.7 million to trade accounts payable and accrued expenses.
In order to allow plans offering enhanced benefits the maximum flexibility in designing alternative
prescription drug coverage, CMS provided a demonstration payment option in lieu of the reinsurance subsidy for
plans offering enhanced coverage, or coverage beyond CMS’s defined standard benefits. The demonstration
payment option is an arrangement in which CMS pays a capitation amount to a plan for assuming the
government’s portion of prescription drug costs in the catastrophic layer of coverage. The capitation amount
represents a fixed monthly amount per member to provide prescription drug coverage in the catastrophic layer.
We chose the demonstration payment option for all of our enhanced benefit plans for 2006 through 2008, but not
for 2009. This capitation amount, derived from our annual bid submissions, is recorded as premium revenue. The
variance between the capitation amount and actual drug costs in the catastrophic layer is subject to risk sharing as
part of the risk corridor settlement.
Settlement of the reinsurance and low-income cost subsidies as well as the risk corridor payment is based on
a reconciliation made approximately 9 months after the close of each calendar year. This reconciliation process
requires us to submit claims data necessary for CMS to administer the program.
59