Humana 2012 Annual Report Download
Download and view the complete annual report
Please find the complete 2012 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
2012
Annual Report
Humana.com
Table of contents
-
Page 1
2012 Annual Report Humana.com -
Page 2
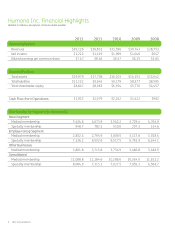
Humana Inc. Financial Highlights (dollars in millions, except per common share results) 2012 Operating Results Revenues Net income Diluted earnings per common share $39,126 $1,222 $7.47 2011 $36,832 $1,419 $8.46 2010 $33,596 $1,099 $6.47 2009 $30,743 $1,040 $6.15 2008 $28,753 $647 $3.83 ... -
Page 3
... and services that incorporate an integrated, holistic approach to lifelong well-being for our 12 million medical and 8 million specialty health plan members nationwide. Humana completed a successful 2012 by enhancing the development of our integrated care delivery model, which we believe represents... -
Page 4
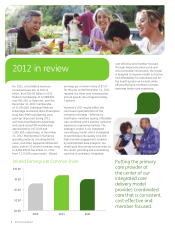
... health care experience. Diluted Earnings per Common Share $10.00 $7.50 $5.00 $2.50 Putting the primary care provider at the center of our integrated care delivery model provides coordinated care that is consistent, cost-effective and member-focused. 2012 $0.00 2010 3 2012 Annual Report 2011 -
Page 5
... HMOs allow our integrated care delivery model to work more effectively for our members than any other plan option. The percentage of individual Medicare Advantage members who chose to enroll in an HMO reached 48 percent during the 2013 Annual Election Period for Medicare beneï¬ciaries in late 2012... -
Page 6
...data-driven information shared among Humana, our providers and our members. The model integrates primary care, home care services, pharmacy services, well-being (including innovative incentives and rewards programs), and data analytics. For our providers, interest in migrating toward a payment model... -
Page 7
...end of 2012, we had approximately 26.5 percent of our individual Medicare Advantage members in such arrangements; our goal is to increase that number to 50 percent by 2017. Grow Medicare membership Expand incentivebased provider contracts Enhance chroniccare capabilities Grow dual-eligible business... -
Page 8
... health system. which includes our three million military members, primarily dependents and retirees, covered through the Department of Defense's TRICARE® program. 7. Achieve additional operating cost efï¬ciencies - By balancing administrative cost management, our focus on strategic initiatives... -
Page 9
... implementation. Humana's long-term belief is that we can greatly improve health care's cost and experience through a model that incorporates ï¬xed payments to providers with aligned incentives, while enabling individuals - through actionable, real-time information - to meet their unique health and... -
Page 10
... Executive Ofï¬cer Ashland Inc. Marissa T. Peterson Former Executive Vice President Worldwide Operations, Services and Customer Advocacy Sun Microsystems, Inc. W. Roy Dunbar Former Chairman of the Board NetworkSolutions David A. Jones, Jr. Chairman Chrysalis Ventures, LLC 9 2012 Annual Report -
Page 11
... STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 10-K Ã ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the fiscal year ended December 31, 2012 OR ' TRANSITION REPORT PURSUANT TO SECTION 13 OR 15 (d) OF THE SECURITIES EXCHANGE ACT... -
Page 12
...Executive Compensation ...Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters ...Certain Relationships and Related Transactions, and Director Independence ...Principal Accounting Fees and Services ...Part IV Item 15. Exhibits, Financial Statement Schedules... -
Page 13
... medical benefit plans, as well as approximately 8.1 million members in our specialty products. During 2012, 75% of our total premiums and services revenue were derived from contracts with the federal government, including 15% derived from our Medicare Advantage contracts in Florida with the Centers... -
Page 14
... marketed directly to individuals. The Employer Group segment consists of Medicare and commercial fully-insured medical and specialty health insurance benefits, including dental, vision, and other supplemental health and financial protection products, as well as administrative services only products... -
Page 15
... persons under the age of 65 certain hospital and medical insurance benefits. CMS, an agency of the United States Department of Health and Human Services, administers the Medicare program. Hospitalization benefits are provided under Part A, without the payment of any premium, for up to 90 days per... -
Page 16
... represented approximately 28% of our individual Medicare Advantage premiums revenue, or 15% of our consolidated premiums and services revenue for the year ended December 31, 2012. Our HMO and PPO products covered under Medicare Advantage contracts with CMS are renewed generally for a calendar year... -
Page 17
... Medicaid benefits, such as nursing home care and/or assistance with Medicare premiums and cost sharing. As of December 31, 2012, we served approximately 285,500 dual eligible members in our Medicare Advantage plans and approximately 697,300 dual eligible members in our stand-alone prescription drug... -
Page 18
...loss insurance coverage from us to cover catastrophic claims or to limit aggregate annual costs. As with individual commercial policies, employers can customize their offerings with optional benefits such as dental, vision, life, and a broad portfolio of financial protection products. Group Medicare... -
Page 19
...$ 1,036 Humana Pharmacy Solutions®, or HPS, manages traditional prescription drug coverage for both individuals and employer groups in addition to providing a broad array of pharmacy solutions. HPS also operates prescription mail order services for brand, generic, and specialty drugs and diabetic... -
Page 20
... sophisticated health-behavior-change model supported by an actuarially sound incentive program. Home care services Home care services include the operations of SeniorBridge Family Companies, Inc., or SeniorBridge, acquired July 6, 2012, and Humana Cares®. As a chronic-care provider of in-home care... -
Page 21
... actual health care costs from an annually negotiated target health care cost. The TRICARE South Region contract represented approximately 93% of total military services premiums and services revenue for the year ended December 31, 2012. Medicaid Medicaid is a federal program that is state-operated... -
Page 22
...cost of long-term care services including those provided by nursing homes, assisted living facilities, and adult day care as well as home health care services. No new policies have been written since 2005 under this closed block. Membership The following table summarizes our total medical membership... -
Page 23
... Medicare healthcare programs applied by the Budget Control Act of 2011. Capitation For some of our medical membership, we share risk with providers under capitation contracts where physicians and hospitals accept varying levels of financial risk for a defined set of membership, primarily HMO. Under... -
Page 24
... most of our commercial, Medicare and Medicaid HMO/POS markets with enough history and membership, except Puerto Rico, and for many of our PPO markets. Sales and Marketing We use various methods to market our products, including television, radio, the Internet, telemarketing, and direct mailings. 14 -
Page 25
..., and make payroll deductions for any premiums payable by the employees. We attempt to become an employer's or group's exclusive source of health insurance benefits by offering a variety of HMO, PPO, and specialty products that provide cost-effective quality health care coverage consistent with the... -
Page 26
... Services We provide centralized management services to each of our health plans and to our business segments from our headquarters and service centers. These services include management information systems, product development and administration, finance, human resources, accounting, law, public... -
Page 27
... to cover services), and various other costs incurred to provide health insurance coverage to our members. These costs also include estimates of future payments to hospitals and others for medical care provided to our members. Generally, premiums in the health care business are fixed for one-year... -
Page 28
...policies including life insurance, annuities, health, and long-term care policies sold to individuals for which some of the premium received in the earlier years is intended to pay anticipated benefits to be incurred in future years. These future policy benefit reserves are recognized on a net level... -
Page 29
.... We are offering both the stand-alone Medicare prescription drug coverage and Medicare Advantage health plan with prescription drug coverage in addition to our other product offerings. We offer the Medicare prescription drug plan in 50 states as well as Puerto Rico and the District of Columbia. The... -
Page 30
... systems-related support, equipment, facilities, and certain data, including data center operations, data network, voice communication services and pharmacy data processing. This dependence makes our operations vulnerable to such third parties' failure to perform adequately under the contract, due... -
Page 31
... premiums; claims relating to the denial of health care benefit payments; claims relating to the denial or rescission of insurance coverage; challenges to the use of some software products used in administering claims; claims relating to our administration of our Medicare Part D offerings; medical... -
Page 32
... Administration, or PRHIA, we provided health insurance coverage to approximately 531,500 Medicaid members in Puerto Rico. These contracts accounted for approximately 2% of our total premiums and services revenue for the year ended December 31, 2012. Effective October 1, 2010, as amended in May 2011... -
Page 33
... provider medical record documentation and coding practices which influence the calculation of premium payments to MA plans. On February 24, 2012, CMS released a "Notice of Final Payment Error Calculation Methodology for Part C Medicare Advantage Risk Adjustment Data Validation (RADV) Contract-Level... -
Page 34
...reductions to the Medicare healthcare programs applied by the Budget Control Act of 2011. We are also subject to various other governmental audits and investigations. Under state laws, our HMOs and health insurance companies are audited by state departments of insurance for financial and contractual... -
Page 35
..., limiting Medicare Advantage payment rates, stipulating a prescribed minimum ratio for the amount of premiums revenue to be expended on medical costs for insured products (and particularly how the ratio may apply to Medicare Advantage and prescription drug plans), additional mandated benefits and... -
Page 36
... revenue, enrollment and premium growth in certain products and market segments, restricting our ability to expand into new markets, increasing our medical and operating costs, lowering our Medicare payment rates and increasing our expenses associated with the nondeductible federal premium tax... -
Page 37
... workers to receive benefits and to appeal benefit denials, prohibit charging medical co-payments or deductibles to employees, may restrict employers' rights to select healthcare providers or direct an injured employee to a specific provider to receive nonemergency workers' compensation medical care... -
Page 38
... (and Puerto Rico) in which we operate our HMOs, PPOs and other health insurance-related services regulate our operations including: licensing requirements, policy language describing benefits, mandated benefits and processes, entry, withdrawal or re-entry into a state or market, rate increases, 28 -
Page 39
delivery systems, utilization review procedures, quality assurance, complaint systems, enrollment requirements, claim payments, marketing, and advertising. The HMO, PPO, and other health insurance-related products we offer are sold under licenses issued by the applicable insurance regulators. Our ... -
Page 40
... payments, or take other actions that could result in higher health care costs for us, less desirable products for customers and members or difficulty meeting regulatory or accreditation requirements. In some markets, some providers, particularly hospitals, physician specialty groups, physician... -
Page 41
... that provide us with purchase discounts and volume rebates on certain prescription drugs dispensed through our mail-order and specialty pharmacies. These discounts and volume rebates are generally passed on to clients in the form of steeper price discounts. Changes in existing federal or state laws... -
Page 42
... payments in our federal and state government health care coverage programs, including the Medicare, military services, and Medicaid programs, and could result in an increase in taxes and assessments on our activities. Although we could attempt to mitigate or cover our exposure from such increased... -
Page 43
... credit rating of the security by the rating agencies; the volatility of the fair value changes; and changes in fair value of the security after the balance sheet date. For debt securities, we take into account expectations of relevant market and economic data. We continuously review our investment... -
Page 44
...outcomes from litigation and government or regulatory investigations; sales of stock by insiders; changes in our credit ratings; limitations on premium levels or the ability to raise premiums on existing policies; increases in minimum capital, reserves, and other financial strength requirements; and... -
Page 45
..., Ohio; and San Juan, Puerto Rico, all of which are used for customer service, enrollment, and claims processing. Our Louisville and Green Bay facilities also house other corporate functions. We own or lease these principal operating facilities in addition to other administrative market offices and... -
Page 46
...matters, claims of medical malpractice, bad faith, nonacceptance or termination of providers, anticompetitive practices, improper rate setting, failure to disclose network discounts and various other provider arrangements, general contractual matters, intellectual property matters, and challenges to... -
Page 47
... of our common stock. Dividends In April 2011, our Board of Directors approved the initiation of a quarterly cash dividend policy. Declaration and payment of future quarterly dividends is at the discretion of the Board and may be adjusted as business needs or market conditions change. The following... -
Page 48
... ("S&P 500") and the Morgan Stanley Health Care Payer Index ("Peer Group") for the five years ended December 31, 2012. The graph assumes an investment of $100 in each of our common stock, the S&P 500, and the Peer Group on December 31, 2007, and that dividends were reinvested when paid. $125 $100... -
Page 49
...10,334,000 11,612,200 Total specialty membership ...8,084,900 7,315,100 7,027,500 7,059,200 6,568,700 (a) Includes the acquired operations of Arcadian Management Services, Inc. from March 31, 2012, SeniorBridge Family Companies, Inc. from July 6, 2012, and Metropolitan Health Networks, Inc. from 39 -
Page 50
... of deferred acquisition costs associated with our individual commercial medical policies and benefits expense of $139 million ($88 million after tax, or $0.52 per diluted common share) associated with reserve strengthening for our closed block of long-term care policies acquired in connection with... -
Page 51
..., marketed directly to individuals. The Employer Group segment consists of Medicare and commercial fullyinsured medical and specialty health insurance benefits, including dental, vision, and other supplemental health and financial protection products, as well as administrative services only products... -
Page 52
.... Comparisons to our 2012 consolidated benefit ratio and operating cost ratio are impacted by the transition to the new TRICARE South Region contract on April 1, 2012, which is accounted for similar to an administrative services fee only agreement as described in our Other Businesses highlights... -
Page 53
... with our agreement with the United States Department of Justice. January 2013 individual Medicare Advantage membership of approximately 2,011,000 increased more than 83,000 members, or approximately 4%, from December 31, 2012, reflecting net membership additions for the 2013 enrollment season and... -
Page 54
...its option to extend the TRICARE South Region contract through March 31, 2014. We account for revenues under the new contract net of estimated health care costs similar to an administrative services fee only agreement. Our previous contract was accounted for similar to our fully-insured products. 44 -
Page 55
... program for those unable to obtain coverage due to a pre-existing condition or health status. Effective January 1, 2011, minimum benefit ratios were mandated for all commercial fully-insured medical plans in the large group (85%), small group (80%), and individual (80%) markets, with annual rebates... -
Page 56
... in which it is payable. The Health Insurance Reform Legislation also specifies benefit design guidelines, limits rating and pricing practices, encourages additional competition (including potential incentives for new market entrants) and expands eligibility for Medicaid programs. In addition, the... -
Page 57
ability to expand into new markets, increasing our medical and operating costs, lowering our Medicare payment rates and increasing our expenses associated with the non-deductible federal premium tax and other assessments; our financial position, including our ability to maintain the value of our ... -
Page 58
... years ended December 31, 2012 and 2011: Consolidated Change 2012 2011 Dollars (dollars in millions, except per common share results) Percentage Revenues: Premiums: Retail ...Employer Group ...Other Businesses ...Total premiums ...Services: Retail ...Employer Group ...Health and Well-Being Services... -
Page 59
..., on April 1, 2012, we began delivering services under the new TRICARE South Region contract that the TMA awarded to us on February 25, 2011. We account for revenues under the new contract net of estimated healthcare costs similar to an administrative services fee only agreement, and as such... -
Page 60
...result of Medicare Advantage growth. The consolidated operating cost ratio for 2012 was 15.1%, increasing 30 basis points from the 2011 operating cost ratio of 14.8% as the negative impact of the new TRICARE South Region contract being accounted for as an administrative services fee only arrangement... -
Page 61
... Humana-Walmart plan offering, supplemented by dual-eligible and age-in enrollments throughout the year. Individual specialty membership increased 166,200, or 21.2%, from December 31, 2011 to December 31, 2012 primarily driven by increased membership in dental offerings. • • Premiums revenue... -
Page 62
... by higher year-overyear clinical, provider, and technological infrastructure spending. Employer Group Segment 2012 2011 Change Members Percentage Membership: Medical membership: Fully-insured commercial group ...1,211,800 ASO ...1,237,700 Group Medicare Advantage ...370,800 Medicare Advantage ASO... -
Page 63
... specialty product sales. • • • Premiums revenue • Employer Group segment premiums increased by $1.3 billion, or 14.2%, from 2011 to $10.1 billion for 2012 primarily due to higher average group Medicare Advantage and fully-insured commercial group medical membership. In addition, 2012... -
Page 64
... priorperiod medical claims reserve development in 2012 than in 2011. These increases were partially offset by the beneficial effect on the benefit ratio in 2012 of a reduction in prior-year premium rebate estimates discussed above. Fully-insured group Medicare Advantage members represented 13... -
Page 65
... Intersegment revenues increased $1.6 billion, or 15.7%, from 2011 to $12.0 billion for 2012 primarily due to growth in our pharmacy solutions business, including our mail-order pharmacy, as it serves our growing membership, particularly Medicare stand-alone PDP. Operating costs • The Health and... -
Page 66
... years ended December 31, 2011 and 2010: Consolidated Change 2011 2010 Dollars (dollars in millions, except per common share results) Percentage Revenues: Premiums: Retail ...Employer Group ...Other Businesses ...Total premiums ...Services: Retail ...Employer Group ...Health and Well-Being Services... -
Page 67
... of long-term care policies in our Other Businesses in 2010 that did not recur in 2011. Year-over-year comparisons of the benefit ratio were negatively impacted by the $62 million decline in favorable prior-period medical claims reserve development from 2010 to 2011. Operating Costs Our segments... -
Page 68
... rate to the effective tax rate. Retail Segment 2011 2010 Change Members Percentage Membership: Medical membership: Individual Medicare Advantage ...Individual Medicare stand-alone PDP ...Total individual Medicare ...Individual commercial ...Total individual medical members ...Individual specialty... -
Page 69
... for the 2011 plan year, supplemented by dual eligible and age-in enrollments throughout the year. Individual specialty membership increased 272,500, or 53.4%, from December 31, 2010 to December 31, 2011 primarily driven by increased sales in dental offerings. • • Premiums revenue • Retail... -
Page 70
... Humana-Walmart plan, first offered in 2011, which carries a higher operating cost ratio than other Medicare products. Employer Group Segment 2011 2010 Change Members Percentage Membership: Medical membership: Fully-insured commercial group ...ASO ...Group Medicare Advantage ...Medicare Advantage... -
Page 71
... Health Insurance Reform Legislation which became effective in 2011, partially offset by an increase in group Medicare Advantage membership. Rebates result in the recognition of lower premiums revenue, as amounts are set aside for payments to commercial customers during the following year. Benefits... -
Page 72
products in 2011. Fully-insured group Medicare Advantage members represented 10.4% of total Employer Group segment medical membership at December 31, 2011 compared to 9.1% at December 31, 2010. The Employer Group segment's pretax income for 2011 included the beneficial effect of $114 million in ... -
Page 73
... closed block of long-term care policies. Excluding this charge, the year-over-year decline primarily reflects a decrease in pretax income associated with our contract with CMS to administer the LI-NET program. Liquidity Our primary sources of cash include receipts of premiums, services revenue, and... -
Page 74
... 2011 and December 31, 2010 primarily consisted of estimated claims owed from the federal government for health care services provided to beneficiaries and underwriting fees under our previous TRICARE South Region contract that expired on March 31, 2012. The claim reimbursement component of military... -
Page 75
... owed to our pharmacy benefit administrator which fluctuate due to bi-weekly payments and the month-end cutoff. (3) Military services benefits payable primarily represents the run-out of the claims liability associated with our previous TRICARE South Region contract that expired on March 31, 2012... -
Page 76
... million less than claim payments during 2011, and $237 million less than claims payments during 2010. Under our new administrative services only TRICARE South Region contract that began April 1, 2012, health care cost payments for which we do not assume risk exceeded reimbursements from the federal... -
Page 77
...October 2012, the Board of Directors declared a cash dividend of $0.26 per share that was paid on January 25, 2013, for an aggregate amount of $42 million, to stockholders of record as of the close of business on December 31, 2012. Stock Repurchase Authorization In April 2012, the Board of Directors... -
Page 78
... of $1.2 billion in 2012, $1.1 billion in 2011, and $747 million in 2010. Refer to our parent company financial statements and accompanying notes in Schedule I - Parent Company Financial Information. As described in Item 7. - Management's Discussion and Analysis of Financial Condition and Results of... -
Page 79
...by these subsidiaries, without prior approval by state regulatory authorities, or ordinary dividends, is limited based on the entity's level of statutory income and statutory capital and surplus. In most states, prior notification is provided before paying a dividend even if approval is not required... -
Page 80
... our total premiums and services revenue for the year ended December 31, 2012, primarily consisted of products covered under the Medicare Advantage and Medicare Part D Prescription Drug Plan contracts with the federal government. These contracts are renewed generally for a calendar year term unless... -
Page 81
...which accounted for approximately 3% of our total premiums and services revenue for the year ended December 31, 2012, primarily consists of contracts in Puerto Rico and Florida, with the vast majority in Puerto Rico. Effective October 1, 2010, as amended in May 2011, the Puerto Rico Health Insurance... -
Page 82
...3,415 339 $3,754 54.8% 10.0% 26.2% 91.0% 9.0% 100.0% Military services benefits payable primarily relates to our previous TRICARE South Region contract that expired on March 31, 2012 and primarily consists of our estimate of incurred healthcare services provided to beneficiaries which were in turn... -
Page 83
... of recent hospital and drug utilization data, provider contracting changes, changes in benefit levels, changes in member cost sharing, changes in medical management processes, product mix, and weekday seasonality. The completion factor method is used for the months of incurred claims prior to the... -
Page 84
... and payment of our benefits payable, excluding military services. Components of the total incurred claims for each year include amounts accrued for current year estimated benefits expense as well as adjustments to prior year estimated accruals. 2012 2011 (in millions) 2010 Balances at January... -
Page 85
... our Medicare Private Fee-For-Service line of business. As a result of these improvements, during 2011 and 2010 we experienced a significant increase in claim overpayment recoveries for claims incurred in prior years, primarily as a result of increased audits of provider billings, as well as system... -
Page 86
... already in payment status remained in such status. Future policy benefits payable was increased to cover future payments to policyholders currently in payment status. Long-term care policies provide for long-duration coverage and, therefore, our actual experience will emerge many years after... -
Page 87
... calendar year minimum benefit ratios for the individual, small group, and large group markets, as defined by the Health Insurance Reform Legislation using a methodology prescribed by the Department of Health and Human Services, separately by state and legal entity. Estimated calendar year rebates... -
Page 88
...premiums revenue or benefits expense for these subsidies or discounts. Receipt and payment activity is accumulated at the contract level and recorded in our consolidated balance sheets in other current assets or trade accounts payable and accrued expenses depending on the contract balance at the end... -
Page 89
... provider networks and clinical programs, claim processing, customer service, enrollment, and other services, while the federal government retains all of the risk of the cost of health benefits. Under the terms of the new TRICARE South Region contract, we do not record premiums revenue or benefits... -
Page 90
...the period services are provided to the customer when the sales price is fixed or determinable, and are net of contractual allowances. The provider reimbursement methods for workers' compensation injury care and related services vary on a state-by-state basis. Most states have fee schedules pursuant... -
Page 91
...defaults and generally provide credit enhancement for bond issues related to our tax-exempt municipal securities. We have no direct exposure to these monoline insurers. We owned $627 million and $634 million at December 31, 2012 and 2011, respectively, of tax-exempt securities guaranteed by monoline... -
Page 92
... a security; payment structure of the security; changes in credit rating of the security by the rating agencies; the volatility of the fair value changes; and changes in fair value of the security after the balance sheet date. For debt securities, we take into account expectations of relevant market... -
Page 93
... the long-term inflation rate. Key assumptions in our cash flow projections, including changes in membership, premium yields, medical and operating cost trends, and certain government contract extensions, are consistent with those utilized in our long-range business plan and annual planning process... -
Page 94
... 31, 2012 and 2011. Our investment portfolio consists of cash, cash equivalents, and investment securities. The modeling technique used to calculate the pro forma net change in pretax earnings considered the cash flows related to fixed income investments and debt, which are subject to interest rate... -
Page 95
...in 2012 and $85 in 2011: ...Other current assets ...Total current assets ...Property and equipment, net ...Long-term investment securities ...Goodwill ...Other long-term assets ...Total assets ...LIABILITIES AND STOCKHOLDERS' EQUITY Current liabilities: Benefits payable ...Trade accounts payable and... -
Page 96
Humana Inc. CONSOLIDATED STATEMENTS OF INCOME For the year ended December 31, 2012 2011 2010 (in millions, except per share results) Revenues: Premiums ...Services ...Investment income ...Total revenues ...Operating expenses: Benefits ...Operating costs ...Depreciation and amortization ...Total ... -
Page 97
Humana Inc. CONSOLIDATED STATEMENTS OF COMPREHENSIVE INCOME For the year ended December 31, 2012 2011 2010 (in millions) Net income ...Other comprehensive income: Gross unrealized investment gain ...Effect of income taxes ...Total unrealized investment gain, net of tax ...Reclassification ... -
Page 98
...stock tax benefit ... 0 17 (1) Balances, December 31, 2010 ...190,245 Net income ...Other comprehensive income ...Common stock repurchases ...Dividends declared ...Stock-based compensation ...Restricted stock grants and restricted stock unit vesting ...11 Restricted stock forfeitures ...(105) Stock... -
Page 99
... year ended December 31, 2012 2011 2010 (in millions) Cash flows from operating activities Net income ...Adjustments to reconcile net income to net cash provided by operating activities: Depreciation and amortization ...Stock-based compensation ...Net realized capital gains ...(Benefit) provision... -
Page 100
... in 2012, including 15% related to our federal government contracts with the Centers for Medicare and Medicaid Services, or CMS, to provide health insurance coverage for Medicare Advantage members in Florida. CMS is the federal government's agency responsible for administering the Medicare program... -
Page 101
... with various state Medicaid programs generally are multi-year contracts subject to annual renewal provisions. Premiums Revenue We bill and collect premium remittances from employer groups and members in our Medicare and other individual products monthly. We receive monthly premiums from the... -
Page 102
... calendar year minimum benefit ratios for the individual, small group, and large group markets, as defined by the Health Insurance Reform Legislation using a methodology prescribed by the Department of Health and Human Services, separately by state and legal entity. Estimated calendar year rebates... -
Page 103
... reimbursements. Instead, we account for revenues under the new contract net of estimated health care costs similar to an administrative services fee only agreement. Our TRICARE members are served by both in-network and out-of-network providers in accordance with the new contract. We pay health care... -
Page 104
... and clinical programs, claim processing, customer service, enrollment, and other services, while the federal government retains all of the risk of the cost of health benefits. We account for revenues under the new contract net of estimated health care costs similar to an administrative services fee... -
Page 105
...-duration employer-group prepaid health services policies typically have a one-year term and may be cancelled upon 30 days notice by the employer group. Life insurance, annuities, health and other supplemental policies sold to individuals are accounted for as long-duration insurance products because... -
Page 106
... our long-lived asset policy. Benefits Payable and Benefits Expense Recognition Benefits expense includes claim payments, capitation payments, pharmacy costs net of rebates, allocations of certain centralized expenses and various other costs incurred to provide health insurance coverage to members... -
Page 107
... any interest-rate swap agreements in 2012, 2011, or 2010. Stock-Based Compensation We generally recognize stock-based compensation expense, as determined on the date of grant at fair value, on a straight-line basis over the period during which an employee is required to provide service in exchange... -
Page 108
... rates generally using a market valuation approach, or, less frequently, an income valuation approach and are generally classified as Level 2. We obtain at least one quoted price for each security from a third party pricing service. These prices are generally derived from recently reported trades... -
Page 109
... of a successful integrated care delivery model that has demonstrated scalability to new markets. A substantial portion of the revenues for both Metropolitan and MCCI are derived from services provided to Humana Medicare Advantage members under capitation contracts with our health plans. In addition... -
Page 110
... customer contracts, trade name, and technology, have a weighted average useful life of 5.2 years. Effective March 31, 2012, we acquired Arcadian Management Services, Inc., or Arcadian, a Medicare Advantage health maintenance organization (HMO) serving members in 15 U.S. states, increasing Medicare... -
Page 111
Humana Inc. NOTES TO CONSOLIDATED FINANCIAL STATEMENTS-(Continued) 4. INVESTMENT SECURITIES Investment securities classified as current and long-term were as follows at December 31, 2012 and 2011, respectively: Amortized Cost Gross Gross Unrealized Unrealized Gains Losses (in millions) Fair Value ... -
Page 112
... across the U.S. with no individual state exceeding 11%. In addition, 20% of our tax-exempt securities were insured by bond insurers and had an equivalent weighted average S&P credit rating of AA- exclusive of the bond insurers' guarantee. Our investment policy limits investments in a single issuer... -
Page 113
... payments. After taking into account these and other factors previously described, we believe these unrealized losses primarily were caused by an increase in market interest rates and tighter liquidity conditions in the current markets than when the securities were purchased. At December 31, 2012... -
Page 114
... December 31, 2012 Cash equivalents ...Debt securities: U.S. Treasury and other U.S. government corporations and agencies: U.S. Treasury and agency obligations ...Mortgage-backed securities ...Tax-exempt municipal securities ...Mortgage-backed securities: Residential ...Commercial ...Asset-backed... -
Page 115
...following: For the years ended December 31, 2011 2010 Private Private Private Placements/ Auction Placements/ Auction Placements/ Auction Venture Rate Venture Rate Venture Rate Capital Securities Total Capital Securities Total Capital Securities Total (in millions) 2012 Beginning balance at January... -
Page 116
...of goodwill for our reportable segments for the years ended December 31, 2012 and 2011 were as follows: Employer Group Health & Well-Being Other Services Businesses (in millions) Retail Total Balance at December 31, 2010 ...Acquisitions ...Subsequent payments/adjustments ...Balance at December 31... -
Page 117
...other long-term assets in the accompanying consolidated balance sheets at December 31, 2012 and 2011: Weighted Average Life 2012 Accumulated Amortization 2011 Accumulated Amortization Cost Net Cost (in millions) Net Other intangible assets: Customer contracts/relationships ...9.5 yrs $ 733 Trade... -
Page 118
... our Medicare Private Fee-For-Service line of business. As a result of these improvements, during 2011 and 2010 we experienced a significant increase in claim overpayment recoveries for claims incurred in prior years, primarily as a result of increased audits of provider billings, as well as system... -
Page 119
... rate for the years ended December 31, 2012, 2011 and 2010 due to the following: 2012 2011 2010 (in millions) Income tax provision at federal statutory rate ...States, net of federal benefit, and Puerto Rico ...Tax exempt investment income ...Nondeductible executive compensation ...Other, net... -
Page 120
... all deferred tax assets. We file income tax returns in the United States and certain foreign jurisdictions. The U.S. Internal Revenue Service, or IRS, has completed its examinations of our consolidated income tax returns for 2011 and prior years. Our 2012 tax return is under advance review by the... -
Page 121
... interest at either LIBOR plus a spread or the base rate plus a spread. The LIBOR spread, currently 120 basis points, varies depending on our credit ratings ranging from 87.5 to 147.5 basis points. We also pay an annual facility fee regardless of utilization. This facility fee, currently 17.5 basis... -
Page 122
... bore a fixed annual interest rate of 8.02% payable quarterly until 2012, and then payable at a floating rate based on LIBOR plus 310 basis points. 12. EMPLOYEE BENEFIT PLANS Employee Savings Plan We have defined contribution retirement savings plans covering eligible employees. Prior to 2011, our... -
Page 123
... retirement-eligible. Upon exercise, stock-based compensation awards are settled with authorized but unissued company stock or treasury stock. The compensation expense that has been charged against income for these plans was as follows for the years ended December 31, 2012, 2011, and 2010: 2012 2011... -
Page 124
... 2011, our Board of Directors approved the initiation of a quarterly cash dividend policy. When valuing employee stock options, we stratify the employee population into three homogenous groups that historically have exhibited similar exercise behaviors. These groups are executive officers, directors... -
Page 125
... are no other contractual terms covering restricted stock once vested. 13. EARNINGS PER COMMON SHARE COMPUTATION Detail supporting the computation of basic and diluted earnings per common share was as follows for the years ended December 31, 2012, 2011 and 2010: 2012 2011 2010 (dollars in millions... -
Page 126
...Board of Directors approved the initiation of a quarterly cash dividend policy. Declaration and payment of future quarterly dividends is at the discretion of the Board and may be adjusted as business needs or market conditions change. The following table provides details of dividend payments in 2011... -
Page 127
...Rent with scheduled escalation terms are accounted for on a straight-line basis over the lease term. Rent expense and sublease rental income, which are recorded net as an operating cost, for all operating leases were as follows for the years ended December 31, 2012, 2011 and 2010: 2012 2011 2010 (in... -
Page 128
... our total premiums and services revenue for the year ended December 31, 2012, primarily consisted of products covered under the Medicare Advantage and Medicare Part D Prescription Drug Plan contracts with the federal government. These contracts are renewed generally for a calendar year term unless... -
Page 129
... 31, 2012, our military services business, which accounted for approximately 3% of our total premiums and services revenue for the year ended December 31, 2012, primarily consisted of the TRICARE South Region contract. On April 1, 2012, we began delivering services under the new TRICARE South Region... -
Page 130
...which accounted for approximately 3% of our total premiums and services revenue for the year ended December 31, 2012, primarily consists of contracts in Puerto Rico and Florida, with the vast majority in Puerto Rico. Effective October 1, 2010, as amended in May 2011, the Puerto Rico Health Insurance... -
Page 131
... and allocate resources. The Retail segment consists of Medicare and commercial fully-insured medical and specialty health insurance benefits, including dental, vision, and other supplemental health and financial protection products, marketed directly to individuals. The Employer Group segment... -
Page 132
...Medicaid, and closed-block long-term care businesses as well as our contract with CMS to administer the LI-NET program. Our Health and Well-Being Services intersegment revenues primarily relate to managing prescription drug coverage for members of our other segments through Humana Pharmacy Solutions... -
Page 133
... 31, 2012, 2011, and 2010: Employer Group Health and Well-Being Other Services Businesses (in millions) Eliminations/ Corporate Retail Consolidated 2012 Revenues-external customers Premiums: Medicare Advantage ...Medicare stand-alone PDP ...Total Medicare ...Fully-insured ...Specialty ...Military... -
Page 134
.../ Services Businesses Corporate Consolidated (in millions) Retail 2011 Revenues-external customers Premiums: Medicare Advantage ...Medicare stand-alone PDP ...Total Medicare ...Fully-insured ...Specialty ...Military services ...Medicaid and other ...Total premiums ...Services revenue: Provider... -
Page 135
.../ Services Businesses Corporate Consolidated (in millions) Retail 2010 Revenues-external customers Premiums: Medicare Advantage ...Medicare stand-alone PDP ...Total Medicare ...Fully-insured ...Specialty ...Military services ...Medicaid and other ...Total premiums ...Services revenue: Provider... -
Page 136
... benefits payable associated with our long-duration insurance products for the years ended December 31, 2012 and 2011. Deferred acquisition costs 2012 2011 Future policy Deferred Future policy benefits acquisition benefits payable costs payable (in millions) Other long-term assets ...Trade accounts... -
Page 137
... policyholders already in payment status remained in such status. Future policy benefits payable was increased to cover future payments to policyholders currently in payment status. During 2010, certain states approved premium rate increases for a large portion of our long-term care block that were... -
Page 138
... (in millions) A.M. Best Rating at December 31, 2012 Protective Life Insurance Company ...Munich American Reassurance Company ...Employers Reassurance Corporation ...General Re Life Corporation ...All others ... $196 78 64 64 59 $461 A+ (superior) A+ (superior) A- (excellent) A++ (superior) A+ to... -
Page 139
... financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (iii) provide reasonable assurance regarding prevention or timely... -
Page 140
Humana Inc. QUARTERLY FINANCIAL INFORMATION (Unaudited) A summary of our quarterly unaudited results of operations for the years ended December 31, 2012 and 2011 follows: 2012 First Second (1) Third Fourth (in millions, except per share results) Total revenues ...Income before income taxes ...Net ... -
Page 141
... reporting is supported by formal policies and procedures which are reviewed, modified and improved as changes occur in business conditions and operations. The Audit Committee of the Board of Directors, which is composed solely of independent outside directors, meets periodically with members... -
Page 142
... over financial reporting as of December 31, 2012 has been audited by PricewaterhouseCoopers LLP, our independent registered public accounting firm, who also audited the Company's consolidated financial statements included in our Annual Report on Form 10-K, as stated in their report which appears... -
Page 143
..., Employer Group Segment Senior Vice President and Chief Human Resources Officer Senior Vice President and Chief Strategy and Corporate Development Officer Senior Vice President and Chief Service and Information Officer President - Retail Segment Senior Vice President - Public Affairs President... -
Page 144
... May 2012. Prior to this, since 2009, Ms. Bierbower led Humana's Specialty Benefits area, including dental, vision, life, disability and workplace voluntary benefits. Ms. Bierbower joined the Company in 2001. (5) Mr. Huval currently serves as Senior Vice President and Chief Human Resources Officer... -
Page 145
...; our Policy Regarding Transactions in Company Securities, Inside Information and Confidentiality; stock ownership guidelines for directors and for executive officers; the Humana Inc. Principles of Business Ethics and any waivers thereto; and the Code of Ethics for the Chief Executive Officer and... -
Page 146
... Equity compensation plan information We maintain plans under which options to purchase our common stock and under which awards of restricted stock may be made to officers, directors, key employees, and consultants. Stock options are granted with an exercise price equal to the fair market value... -
Page 147
... Annual Meeting of Stockholders scheduled to be held on April 25, 2013 appearing under the captions "Certain Transactions with Management and Others" and "Corporate Governance - Independent Directors" of such Proxy Statement. ITEM 14. PRINCIPAL ACCOUNTING FEES AND SERVICES The information required... -
Page 148
...Other long-term indebtedness of Humana Inc. is described herein in Note 11 to Consolidated Financial Statements. Humana Inc. agrees to furnish copies of all such instruments defining the rights of the holders of such indebtedness not otherwise filed as an Exhibit to this Annual Report on Form 10K to... -
Page 149
...Trust under Humana Inc. Deferred Compensation Plans (incorporated herein by reference to Exhibit 10(p) to Humana Inc.'s Annual Report on Form 10-K for the fiscal year ended December 31, 1999). The Humana Inc. Deferred Compensation Plan for Non-Employee Directors (as amended on October 18, 2012). 139... -
Page 150
... February 17, 2011). Letter agreement with Humana Inc. officers concerning health insurance availability (incorporated herein by reference to Exhibit 10(mm) to Humana Inc.'s Annual Report on Form 10-K for the fiscal year ended December 31, 1994). Executive Long-Term Disability Program (incorporated... -
Page 151
... Department of Defense and Humana Military Healthcare Services, Inc., a wholly owned subsidiary of Humana Inc., dated as March 3, 2011 (incorporated herein by reference to Exhibit 10(mm) to Humana Inc.'s Annual Report on Form 10-K filed on February 24, 2012). Humana Inc. 2011 Stock Incentive Plan... -
Page 152
...Extensible Business Reporting Language): (i) the Consolidated Balance Sheets at December 31, 2012 and 2011; (ii) the Consolidated Statements of Income for the years ended December 31, 2012, 2011 and 2010; (iii) the Consolidated Statements of Comprehensive Income for the years ended December 31, 2012... -
Page 153
Humana Inc. SCHEDULE I-PARENT COMPANY FINANCIAL INFORMATION CONDENSED BALANCE SHEETS December 31, 2012 2011 (in millions, except share amounts) ASSETS Current assets: Cash and cash equivalents ...Investment securities ...Receivable from operating subsidiaries ...Other current assets ...Total ... -
Page 154
Humana Inc. SCHEDULE I-PARENT COMPANY FINANCIAL INFORMATION CONDENSED STATEMENTS OF INCOME For the year ended December 31, 2012 2011 2010 (in millions) Revenues: Management fees charged to operating subsidiaries ...Investment and other income, net ...Expenses: Operating costs ...Depreciation ...... -
Page 155
Humana Inc. SCHEDULE I-PARENT COMPANY FINANCIAL INFORMATION CONDENSED STATEMENTS OF COMPREHENSIVE INCOME For the year ended December 31, 2012 2011 2010 (in millions) Net income ...Other comprehensive income: Gross unrealized investment gain ...Effect of income taxes ...Total unrealized investment ... -
Page 156
...SCHEDULE I-PARENT COMPANY FINANCIAL INFORMATION CONDENSED STATEMENTS OF CASH FLOWS For the year ended December 31, 2012 2011 2010 (in millions) Net cash provided by operating activities ...Cash flows from investing activities: Acquisitions ...Purchases of investment securities ...Proceeds from sale... -
Page 157
...parent company, charges a management fee for reimbursement of certain centralized services provided to its subsidiaries including information systems, disbursement, investment and cash administration, marketing, legal, finance, and medical and executive management oversight. Dividends Cash dividends... -
Page 158
Humana Inc. SCHEDULE I-PARENT COMPANY FINANCIAL INFORMATION NOTES TO CONDENSED FINANCIAL STATEMENTS-(Continued) Although minimum required levels of equity are largely based on premium volume, product mix, and the quality of assets held, minimum requirements vary significantly at the state level. Our... -
Page 159
Humana Inc. SCHEDULE II-VALUATION AND QUALIFYING ACCOUNTS For the Years Ended December 31, 2012, 2011, and 2010 (in millions) Additions Charged (Credited) to Charged to Costs and Other Expenses Accounts (1) Balance at Beginning of Period Acquired Balances Deductions or Write-offs Balance at End ... -
Page 160
..., thereto duly authorized. HUMANA INC. By: /S/ JAMES H. BLOEM James H. Bloem Senior Vice President, Chief Financial Officer and Treasurer (Principal Financial Officer) Date: February 21, 2013 Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed... -
Page 161
[THIS PAGE INTENTIONALLY LEFT BLANK] -
Page 162
[THIS PAGE INTENTIONALLY LEFT BLANK] -
Page 163
... 40201-1438 Transfer Agent and Registrar American Stock Transfer & Trust Company, LLC Shareholder Services - ATTN: Operations Center 6201 15th Avenue Brooklyn, New York 11219 800.937.5449 Shareholder Services Direct Dial: 718.921.8124 www.amstock.com Email: [email protected] 2012 Annual Report 10 -
Page 164
Humana.com 4 2012 Annual Report GCHHHQBHH