Humana 2012 Annual Report Download - page 87
Download and view the complete annual report
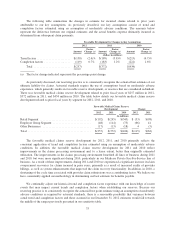
Please find page 87 of the 2012 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.approved premium rate increases for a large portion of our long-term care block that were significantly below our
acquisition date assumptions. Based on these actions by the states, combined with lower interest rates and higher
actual expenses as compared to acquisition date assumptions, we determined that our existing future policy
benefits payable, together with the present value of future gross premiums, associated with our long-term care
policies were not adequate to provide for future policy benefits under these policies; therefore we unlocked and
modified our assumptions based on current expectations. Accordingly, during 2010 we recorded $139 million of
additional benefits expense, with a corresponding increase in future policy benefits payable of $170 million
partially offset by a related reinsurance recoverable of $31 million included in other long-term assets. In addition,
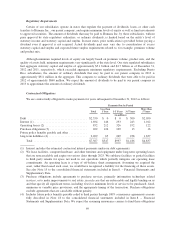
future policy benefits payable include amounts of $220 million at December 31, 2012 and of $224 million at
December 31, 2011 which are subject to 100% coinsurance agreements as more fully described in Note 18 to the
consolidated financial statements included in Item 8. – Financial Statements and Supplementary Data, and as
such are offset by a related reinsurance recoverable included in other long-term assets.
Revenue Recognition
We generally establish one-year commercial membership contracts with employer groups, subject to
cancellation by the employer group on 30-day written notice. Our Medicare contracts with CMS renew annually.
Our military services contracts with the federal government and our contracts with various state Medicaid
programs generally are multi-year contracts subject to annual renewal provisions.
Our commercial contracts establish rates on a per employee basis for each month of coverage based on the
type of coverage purchased (single to family coverage options). Our Medicare and Medicaid contracts also
establish monthly rates per member. However, our Medicare contracts also have additional provisions as outlined
in the following separate section.
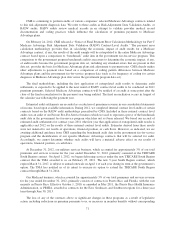
Premiums revenue and administrative services only, or ASO, fees are estimated by multiplying the
membership covered under the various contracts by the contractual rates. In addition, we adjust revenues for
estimated changes in an employer’s enrollment and individuals that ultimately may fail to pay, and beginning
January 1, 2011, for estimated rebates to policyholders under the minimum benefit ratios required under the
Health Insurance Reform Legislation. We estimate these policyholder rebates by projecting calendar year
minimum benefit ratios for the individual, small group, and large group markets, as defined by the Health
Insurance Reform Legislation using a methodology prescribed by the Department of Health and Human Services,
separately by state and legal entity. Estimated calendar year rebates recognized ratably during the year are
revised each period to reflect current experience. Enrollment changes not yet processed or not yet reported by an
employer group or the government, also known as retroactive membership adjustments, are estimated based on
available data and historical trends. We routinely monitor the collectibility of specific accounts, the aging of
receivables, historical retroactivity trends, estimated rebates, as well as prevailing and anticipated economic
conditions, and reflect any required adjustments in the current period’s revenue.
We bill and collect premium remittances from employer groups and members in our Medicare and other
individual products monthly. We receive monthly premiums from the federal government and various states
according to government specified payment rates and various contractual terms. Changes in revenues from CMS
for our Medicare products resulting from the periodic changes in risk-adjustment scores derived from medical
diagnoses for our membership are recognized when the amounts become determinable and the collectibility is
reasonably assured.
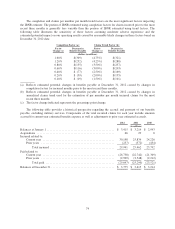
Medicare Part D Provisions
We cover prescription drug benefits in accordance with Medicare Part D under multiple contracts with
CMS. The payments we receive monthly from CMS and members, which are determined from our annual bid,
represent amounts for providing prescription drug insurance coverage. We recognize premiums revenue for
providing this insurance coverage ratably over the term of our annual contract. Our CMS payment is subject to
77