Humana 2012 Annual Report Download - page 81
Download and view the complete annual report
Please find page 81 of the 2012 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.CMS is continuing to perform audits of various companies’ selected Medicare Advantage contracts related
to this risk adjustment diagnosis data. We refer to these audits as Risk-Adjustment Data Validation Audits, or
RADV audits. RADV audits review medical records in an attempt to validate provider medical record
documentation and coding practices which influence the calculation of premium payments to Medicare
Advantage plans.
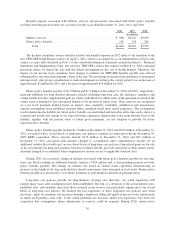
On February 24, 2012, CMS released a “Notice of Final Payment Error Calculation Methodology for Part C
Medicare Advantage Risk Adjustment Data Validation (RADV) Contract-Level Audits.” The payment error
calculation methodology provides that, in calculating the economic impact of audit results for a Medicare
Advantage contract, if any, the results of the audit sample will be extrapolated to the entire Medicare Advantage
contract based upon a comparison to “benchmark” audit data in the government fee-for-service program. This
comparison to the government program benchmark audit is necessary to determine the economic impact, if any,
of audit results because the government program data set, including any attendant errors that are present in that
data set, provides the basis for Medicare Advantage plans risk adjustment to payment rates. CMS already makes
other adjustments to payment rates based on a comparison of coding pattern differences between Medicare
Advantage plans and the government fee-for-service program data (such as for frequency of coding for certain
diagnoses in Medicare Advantage plan data versus the government program data set).
The final methodology, including the first application of extrapolated audit results to determine audit
settlements, is expected to be applied to the next round of RADV contract level audits to be conducted on 2011
premium payments. Selected Medicare Advantage contracts will be notified of an audit at some point after the
close of the final reconciliation for the payment year being audited. The final reconciliation occurs in August of
the calendar year following the payment year.
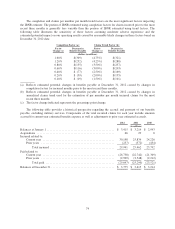
Estimated audit settlements are recorded as a reduction of premiums revenue in our consolidated statements
of income, based upon available information. During 2012, we completed internal contract level audits of certain
contracts based on the RADV audit methodology prescribed by CMS. Included in these internal contract level
audits was an audit of our Private Fee-For-Service business which we used to represent a proxy of the benchmark
audit data in the government fee-for-service program which has not yet been released. We based our accrual of
estimated audit settlements for contract years 2011 (the first year that application of extrapolated audit results is
applicable) and 2012 on the results of these internal contract level audits. Estimates derived from these results
were not material to our results of operations, financial position, or cash flows. However, as indicated, we are
awaiting additional guidance from CMS regarding the benchmark audit data in the government fee-for-service
program and the identification of our specific Medicare Advantage contracts that will be selected for audit.
Accordingly, we cannot determine whether such audits will have a material adverse effect on our results of
operations, financial position, or cash flows.
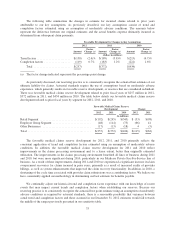
At December 31, 2012, our military services business, which accounted for approximately 3% of our total
premiums and services revenue for the year ended December 31, 2012, primarily consisted of the TRICARE
South Region contract. On April 1, 2012, we began delivering services under the new TRICARE South Region
contract that the TMA awarded to us on February 25, 2011. The new 5-year South Region contract, which
expires March 31, 2017, is subject to annual renewals on April 1 of each year during its term at the government’s
option. The TMA has notified us of its intent to exercise its option to extend the TRICARE South Region
contract through March 31, 2014.
Our Medicaid business, which accounted for approximately 3% of our total premiums and services revenue
for the year ended December 31, 2012, primarily consists of contracts in Puerto Rico and Florida, with the vast
majority in Puerto Rico. Effective October 1, 2010, as amended in May 2011, the Puerto Rico Health Insurance
Administration, or PRHIA, awarded us contracts for the East, Southeast, and Southwest regions for a three-year
term through June 30, 2013.
The loss of any of the contracts above or significant changes in these programs as a result of legislative
action, including reductions in premium payments to us, or increases in member benefits without corresponding
71