Humana 2012 Annual Report Download - page 130
Download and view the complete annual report
Please find page 130 of the 2012 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Humana Inc.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Our Medicaid business, which accounted for approximately 3% of our total premiums and services revenue
for the year ended December 31, 2012, primarily consists of contracts in Puerto Rico and Florida, with the vast
majority in Puerto Rico. Effective October 1, 2010, as amended in May 2011, the Puerto Rico Health Insurance
Administration, or PRHIA, awarded us contracts for the East, Southeast, and Southwest regions for a three-year
term through June 30, 2013.
The loss of any of the contracts above or significant changes in these programs as a result of legislative
action, including reductions in premium payments to us, or increases in member benefits without corresponding
increases in premium payments to us, may have a material adverse effect on our results of operations, financial
position, and cash flows.
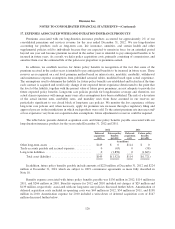
Legal Proceedings and Certain Regulatory Matters
Florida Matters
On December 16, 2010, an individual filed a qui tam suit captioned United States of America ex rel. Marc
Osheroff v. Humana et al. in the Southern District of Florida, against us, several of our health plan subsidiaries,
and certain other companies that operate medical centers in Miami-Dade County, Florida. After the U.S.
government declined to intervene, the Court ordered the complaint unsealed, and the individual plaintiff amended
his complaint and served the Company on December 8, 2011. The amended complaint alleges certain civil
violations by our CAC Medical Centers in Florida, including offering various amenities such as transportation
and meals, to Medicare and dual eligible individuals in our community center settings. The amended complaint
also alleges civil violations by our Medicare Advantage health plans in Florida, arising from the alleged activities
of our CAC Medical Centers and the codefendants in the complaint. The amended complaint seeks damages and
penalties on behalf of the United States under the Anti-Inducement and Anti-Kickback Statutes and the False
Claims Act. On September 28, 2012, the Court dismissed, with prejudice, all causes of action that were asserted
in the suit. On January 31, 2013, the Court denied a motion for reconsideration filed by the individual plaintiff.
We expect the individual plaintiff to appeal the Court’s ruling.
On January 6, 2012, the Civil Division of the United States Attorney’s Office for the Southern District of
Florida advised our legal counsel that it is seeking documents and information from us and several of our
affiliates relating to several matters including the coding of medical claims by one or more South Florida medical
providers, and loans to physician practices.
Other Lawsuits and Regulatory Matters
Our current and past business practices are subject to review or other investigations by various state
insurance and health care regulatory authorities and other state and federal regulatory authorities. These
authorities regularly scrutinize the business practices of health insurance and benefits companies. These reviews
focus on numerous facets of our business, including claims payment practices, provider contracting, competitive
practices, commission payments, privacy issues, utilization management practices, and sales practices, among
others. Some of these reviews have historically resulted in fines imposed on us and some have required changes
to some of our practices. We continue to be subject to these reviews, which could result in additional fines or
other sanctions being imposed on us or additional changes in some of our practices.
We also are involved in various other lawsuits that arise, for the most part, in the ordinary course of our
business operations, certain of which may be styled as class-action lawsuits. Among other matters, this litigation
may include employment matters, claims of medical malpractice, bad faith, nonacceptance or termination of
providers, anticompetitive practices, improper rate setting, failure to disclose network discounts and various other
120