Humana 2006 Annual Report Download - page 34
Download and view the complete annual report
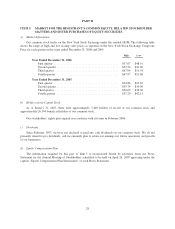
Please find page 34 of the 2006 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.reinsurance claim. In addition, in the event the settlement represents an amount CMS owes us, there is a
negative impact on our cash flows and financial condition as a result of financing CMS’s share of the
risk. The opposite is true in the event the settlement represents an amount we owe CMS;
• future changes to these government programs which may affect our ability or willingness to participate
in these programs;
• higher comparative medical costs;
• government regulatory and reporting requirements; and
• higher marketing and advertising costs per member as a result of marketing to individuals as opposed to
groups.
Our industry is currently subject to substantial government regulation, which, along with possible
increased governmental regulation or legislative reform, increases our costs of doing business and could
adversely affect our profitability.
The health care industry in general, and health insurance, particularly HMOs and PPOs are subject to
substantial federal and state government regulation.
Our licensed subsidiaries are subject to regulation under state insurance holding company and Puerto Rico
regulations. These regulations generally require, among other things, prior approval and/or notice of new
products, rates, benefit changes, and certain material transactions, including dividend payments, purchases or
sales of assets, intercompany agreements, and the filing of various financial and operational reports.
Certain of our subsidiaries operate in states that regulate the payment of dividends, loans, or other cash
transfers to Humana Inc., our parent company, and require minimum levels of equity as well as limit investments
to approved securities. The amount of dividends that may be paid to Humana Inc. by these subsidiaries, without
prior approval by state regulatory authorities, is limited based on the entity’s level of statutory income and
statutory capital and surplus. In most states, prior notification is provided before paying a dividend even if
approval is not required.
As of December 31, 2006, we maintained aggregate statutory capital and surplus of $2,066.0 million in our
state regulated subsidiaries. Each of these subsidiaries was in compliance with applicable statutory requirements
which aggregated $1,430.3 million. Although the minimum required levels of equity are largely based on
premium volume, product mix, and the quality of assets held, minimum requirements can vary significantly at
the state level. Given our anticipated continued premium growth in 2007, capital requirements will increase. We
expect to fund these increased requirements with capital contributions from Humana Inc., our parent company, in
the range of $325 million to $425 million in 2007.
Most states rely on risk-based capital requirements, or RBC, to define their required levels of equity
discussed above. RBC is a model developed by the National Association of Insurance Commissioners to monitor
an entity’s solvency. This calculation indicates recommended minimum levels of required capital and surplus and
signals regulatory measures should actual surplus fall below these recommended levels. If RBC were adopted by
the remaining states and Puerto Rico at December 31, 2006, each of our subsidiaries would be in substantial
compliance and we would have $516.2 million of aggregate capital and surplus above any of the levels that
require corrective action under RBC, or individual state requirements.
The use of individually identifiable health data by our business is regulated at federal and state levels. These
laws and rules are changed frequently by legislation or administrative interpretation. Various state laws address
the use and maintenance of individually identifiable health data. Most are derived from the privacy provisions in
the federal Gramm-Leach-Bliley Act and HIPAA. HIPAA includes administrative provisions directed at
simplifying electronic data interchange through standardizing transactions, establishing uniform health care
provider, payer, and employer identifiers and seeking protections for confidentiality and security of patient data.
22