Humana 2006 Annual Report Download - page 69
Download and view the complete annual report
Please find page 69 of the 2006 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
CMS has transitioned to the risk adjustment model while the old demographic model was phased out. The
demographic model based the monthly premiums paid to health plans on factors such as age, sex and disability
status. The monthly premium amount for each member is separately determined under both the risk adjustment
and demographic model. These separate payment amounts are then blended according to the transition schedule.
CMS transitioned to the risk adjustment model for Medicare Advantage plans as follows: 30% in 2004, 50% in
2005, 75% in 2006 and 100% in 2007. The stand-alone PDP payment methodology is based 100% on the risk
adjustment model. As a result of this process and the phasing in of the risk adjustment model, as well as budget
neutrality as described on page 5, our CMS monthly premium payments per member may change materially,
either favorably or unfavorably.
TRICARE Contract
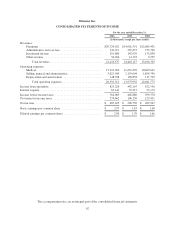
In 2006, TRICARE revenues represented 12% of total premiums and administrative services fees. The
single TRICARE contract for the South Region includes multiple revenue generating activities and as such was
evaluated under Emerging Issues Task Force (EITF) Issue No. 00-21, Accounting for Revenue Arrangements
with Multiple Deliverables. We allocate the consideration to the various components based on the relative fair
values of the components. TRICARE revenues consist generally of (1) an insurance premium for assuming
underwriting risk for the cost of civilian health care services delivered to eligible beneficiaries; (2) health care
services provided to beneficiaries which are in turn reimbursed by the federal government; and (3) ASO fees
related to claim processing, customer service, enrollment, disease management and other services. We recognize
the insurance premium as revenue ratably over the period coverage is provided. Health care services
reimbursements are recognized as revenue in the period health care services are provided. Administrative service
fees are recognized as revenue in the period services are performed.
The TRICARE contract contains provisions whereby the federal government bears a substantial portion of
the risk associated with financing the cost of health benefits. Annually, we negotiate a target health care cost
amount, or target cost, with the federal government and determine an underwriting fee. Any variance from the
target cost is shared. We earn more revenue or incur additional costs based on the variance in actual health care
costs versus the negotiated target cost. We receive 20% for any cost underrun, subject to a ceiling that limits the
underwriting profit to 10% of the target cost. We pay 20% for any cost overrun, subject to a floor that limits the
underwriting loss to negative 4% of the target cost. A final settlement occurs 12 to 18 months after the end of
each contract year to which it applies. We defer the recognition of any revenues for favorable contingent
underwriting fee adjustments related to cost underruns until the amount is determinable and the collectibility is
reasonably assured. We estimate and recognize unfavorable contingent underwriting fee adjustments related to
cost overruns currently in operations as an increase in medical expenses. We continually review these medical
expense estimates of future payments to the government for cost overruns and make necessary adjustments to our
reserves.
The TRICARE contract contains provisions to negotiate change orders. Change orders occur when we
perform services or incur costs under the directive of the federal government that were not originally specified in
our contract. Under federal regulations we may be entitled to an equitable adjustment to the contract price in
these situations. Change orders may be negotiated and settled at any time throughout the year. We record revenue
applicable to change orders when services are performed and these amounts are determinable and the
collectibility is reasonably assured.
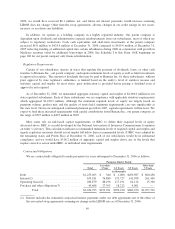
Investment Securities
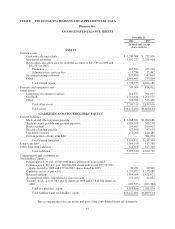
Investment securities totaled $3,607.2 million, or 36% of total assets at December 31, 2006. Debt securities
totaled $3,598.3 million, or 99% of this investment portfolio. More than 97% of our debt securities were of
investment-grade quality, with an average credit rating of AA+ by S&P at December 31, 2006. Most of the debt
securities that are below investment grade are rated at the higher end (BB or better) of the non-investment grade
spectrum. Our investment policy limits investments in a single issuer and requires diversification among various
asset types.
57