Humana 2006 Annual Report Download - page 79
Download and view the complete annual report
Please find page 79 of the 2006 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Humana Inc.
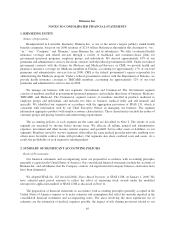
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Receivables and Revenue Recognition
We generally establish one-year commercial membership contracts with employer groups, subject to
cancellation by the employer group on 30-day written notice. Our TRICARE contract with the federal
government and our contracts with various state Medicaid programs generally are multi-year contracts subject to
annual renewal provisions. Our Medicare contracts with CMS renew annually.
We bill and collect premium and administrative fee remittances from employer groups and members in our
Medicare and individual products monthly. We receive monthly premiums and administrative fees from the
federal government and various states according to government specified reimbursement rates and various
contractual terms. Changes in revenues from CMS for our Medicare products resulting from the periodic changes
in risk adjustment scores for our membership are recognized when the amounts become determinable and the
collectibility is reasonably assured.
Premium revenues are recognized as income in the period members are entitled to receive services, and are
net of estimated uncollectible amounts and retroactive membership adjustments. Retroactive membership
adjustments result from enrollment changes not yet processed, or not yet reported by an employer group or the
government. We routinely monitor the collectibility of specific accounts, the aging of receivables, historical
retroactivity trends, as well as prevailing and anticipated economic conditions, and reflect any required
adjustments in current operations.
Medicare Part D
On January 1, 2006, we began covering prescription drug benefits in accordance with Medicare Part D
under multiple contracts with CMS. The payments we receive monthly from CMS and members, which are
determined from our annual bid, represent amounts for providing prescription drug insurance coverage. We
recognize premium revenues for providing this insurance coverage ratably over the term of our annual contract.
Our CMS payment is subject to risk sharing through the Medicare Part D risk corridor provisions. In addition,
receipts for reinsurance and low-income cost subsidies represent reimbursements of prescription drug costs for
which we are not at risk.
The risk corridor provisions compare costs targeted in our bids to actual prescription drug costs, limited to
actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding
certain thresholds may result in CMS making additional payments to us or require us to refund to CMS a portion
of the premiums we received. We estimate and recognize an adjustment to premium revenues related to these risk
corridor provisions based upon pharmacy claims experience to date as if the annual contract were to terminate at
the end of the reporting period. Accordingly, this estimate provides no consideration to future pharmacy claims
experience. We record a receivable or payable at the contract level and classify the amount as current or long-
term in the consolidated balance sheets based on the expected settlement.
Reinsurance and low-income cost subsidies represent reimbursements from CMS in connection with the
Medicare Part D program for which we assume no risk. Reinsurance subsidies represent reimbursements for CMS’s
portion of prescription drug costs which exceed the member’s out-of-pocket threshold, or the catastrophic coverage
level. Low-income cost subsidies represent reimbursements from CMS for all or a portion of the deductible, the
coinsurance and co-payment amounts above the out-of-pocket threshold for low-income beneficiaries. Monthly
prospective payments from CMS for reinsurance and low-income cost subsidies are based on assumptions
submitted with our annual bid. A reconciliation and related settlement of CMS’s prospective subsidies against
actual prescription drug costs we paid is made after the end of the year. We account for these subsidies as a deposit
in our consolidated balance sheets and as a financing activity in our consolidated statements of cash flows. We do
not recognize premium revenues or claims expense for these subsidies. Receipt and payment activity is accumulated
67