Humana 2009 Annual Report Download - page 15
Download and view the complete annual report
Please find page 15 of the 2009 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Our Products Marketed to Government Segment Members and Beneficiaries
Medicare
We have participated in the Medicare program for private health plans for over 20 years and have
established a national presence, offering at least one type of Medicare plan in all 50 states. The resulting growing
membership base provides us with greater ability to expand our network of PPO and HMO providers. We
employ strategies including health assessments and clinical guidance programs such as lifestyle and fitness
programs for seniors to guide Medicare beneficiaries in making cost-effective decisions with respect to their
health care, including cost savings that occur from making positive behavior changes that result in living
healthier.
Medicare is a federal program that provides persons age 65 and over and some disabled persons under the
age of 65 certain hospital and medical insurance benefits. Hospitalization benefits are provided under Part A,
without the payment of any premium, for up to 90 days per incident of illness plus a lifetime reserve aggregating
60 days. Eligible beneficiaries are required to pay an annually adjusted premium to the federal government to be
eligible for physician care and other services under Part B. Beneficiaries eligible for Part A and Part B coverage
under traditional Medicare are still required to pay out-of-pocket deductibles and coinsurance. Prescription drug
benefits are provided under Part D. CMS, an agency of the United States Department of Health and Human
Services, administers the Medicare program.
Medicare Advantage Products
We contract with CMS under the Medicare Advantage program to provide a comprehensive array of health
insurance benefits, including wellness programs, to Medicare eligible persons under HMO, PPO, and PFFS plans
in exchange for contractual payments received from CMS, usually a fixed payment per member per month. With
each of these products, the beneficiary receives benefits in excess of original Medicare, typically including
reduced cost sharing, enhanced prescription drug benefits, care coordination, data analysis techniques to help
identify member needs, complex case management, tools to guide members in their health care decisions, disease
management programs, wellness and prevention programs and, in some instances, a reduced monthly Part B
premium. Since 2006, Medicare beneficiaries have had more health plan options, including a prescription drug
benefit option. Most Medicare Advantage plans offer the prescription drug benefit under Part D as part of the
basic plan, subject to cost sharing and other limitations. Accordingly, all of the provisions of the Medicare Part D
program described in connection with our stand-alone prescription drug plans in the following section also are
applicable to most of our Medicare Advantage plans. Medicare Advantage plans may charge beneficiaries
monthly premiums and other copayments for Medicare-covered services or for certain extra benefits.
Our Medicare HMO and PPO plans, which cover Medicare-eligible individuals residing in certain counties,
may eliminate or reduce coinsurance or the level of deductibles on many other medical services while seeking
care from participating in-network providers or in emergency situations. Except in emergency situations, HMO
plans provide no out-of-network benefits. PPO plans carry an out-of network benefit that is subject to higher
member cost-sharing. In most cases, these beneficiaries are required to pay a monthly premium to the HMO or
PPO plan in addition to the monthly Part B premium they are required to pay the Medicare program.
Our Medicare PFFS plans generally have no preferred network. Individuals in these plans pay us a monthly
premium to receive typical Medicare Advantage benefits along with the freedom to choose any health care
provider that accepts individuals at rates equivalent to traditional Medicare payment rates.
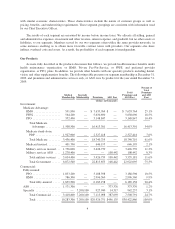
CMS uses monthly rates per person for each county to determine the fixed monthly payments per member to
pay to health benefit plans. These rates are adjusted under CMS’s risk-adjustment model which uses health status
indicators, or risk scores, to improve the adequacy of payment. The risk-adjustment model, which CMS
implemented pursuant to the Balanced Budget Act of 1997 (BBA) and the Benefits and Improvement Protection
Act of 2000 (BIPA), generally pays more for members with predictably higher costs and uses principal hospital
5