Humana 2009 Annual Report Download - page 16
Download and view the complete annual report
Please find page 16 of the 2009 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.inpatient diagnoses as well as diagnosis data from ambulatory treatment settings (hospital outpatient department
and physician visits). CMS transitioned to this risk-based payment model while the old payment model based on
demographic data including gender, age, and disability status was phased out. The phase-in of risk adjusted
payment was completed in 2007. Under the risk-adjustment methodology, all health benefit organizations must
collect and submit the necessary diagnosis code information to CMS within prescribed deadlines.
Commensurate with the phase-in of the risk-adjustment methodology, payments to Medicare Advantage
plans were increased by a “budget neutrality” factor. The budget neutrality factor was implemented to prevent
overall health plan payments from being reduced during the transition from the previous payment model, based
upon average original Medicare fee-for-service spending, to the risk-adjustment payment model. The budget
neutrality adjustment began phasing out in 2007 and will be fully eliminated by 2011.
At December 31, 2009, we provided health insurance coverage under CMS contracts to approximately
1,508,500 Medicare Advantage members for which we received premium revenues of approximately $16.4
billion, or 54.0%, of our total premiums and ASO fees for the year ended December 31, 2009. Under our
Medicare Advantage contracts with CMS in Florida, we provided health insurance coverage to approximately
377,900 members. These contracts accounted for premium revenues of approximately $5.2 billion, which
represented approximately 31.8% of our Medicare Advantage premium revenues, or 17.1% of our total premiums
and ASO fees for the year ended December 31, 2009.
Our HMO, PFFS, and PPO products covered under Medicare Advantage contracts with CMS are renewed
generally for a one-year term each December 31 unless CMS notifies us of its decision not to renew by August 1
of the year in which the contract would end, or we notify CMS of our decision not to renew by the first Monday
in June of the year in which the contract would end. All material contracts between Humana and CMS relating to
our Medicare Advantage business have been renewed for 2010.
Medicare Stand-Alone Prescription Drug Products
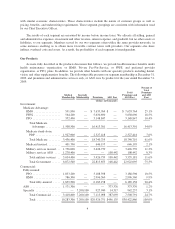
We offer stand-alone prescription drug plans, or PDPs, under Medicare Part D. Generally, Medicare-eligible
individuals enroll in one of our plan choices between November 15 and December 31 for coverage that begins
January 1. Our stand-alone PDP offerings consist of plans offering basic coverage with benefits mandated by
Congress, as well as plans providing enhanced coverage with varying degrees of out-of-pocket costs for
premiums, deductibles and co-insurance. Our revenues from CMS and the beneficiary are determined from our
bids submitted annually to CMS. These revenues also reflect the health status of the beneficiary and risk sharing
provisions as more fully described beginning on page 60. Our stand-alone PDP contracts with CMS are renewed
generally for a one-year term each December 31 unless CMS notifies us of its decision not to renew by August 1
of the year in which the contract would end, or we notify CMS of our decision not to renew by the first Monday
in June of the year in which the contract would end. All material contracts between Humana and CMS relating to
our Medicare stand-alone PDP business have been renewed for 2010.
Medicare stand-alone PDP premium revenues were approximately $2.3 billion, or 7.6% of our total
premiums and ASO fees for the year ended December 31, 2009.
Medicaid Product
Medicaid is a federal program that is state-operated to facilitate the delivery of health care services
primarily to low-income residents. Each electing state develops, through a state-specific regulatory agency, a
Medicaid managed care initiative that must be approved by CMS. CMS requires that Medicaid managed care
plans meet federal standards and cost no more than the amount that would have been spent on a comparable
fee-for-service basis. States currently either use a formal proposal process in which they review many bidders
before selecting one or award individual contracts to qualified bidders who apply for entry to the program. In
either case, the contractual relationship with a state generally is for a one-year period. Under these contracts, we
6