Humana 2009 Annual Report Download - page 70
Download and view the complete annual report
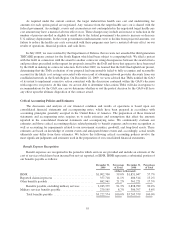
Please find page 70 of the 2009 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Premium revenues and ASO fees are estimated by multiplying the membership covered under the various
contracts by the contractual rates. In addition, we adjust revenues for estimated changes in an employer’s
enrollment and individuals that ultimately may fail to pay. Enrollment changes not yet processed or not yet
reported by an employer group or the government, also known as retroactive membership adjustments, are
estimated based on available data and historical trends. We routinely monitor the collectibility of specific
accounts, the aging of receivables, historical retroactivity trends, as well as prevailing and anticipated economic
conditions, and reflect any required adjustments in the current period’s revenue.
We bill and collect premium and administrative fee remittances from employer groups and members in our
Medicare and individual products monthly. We receive monthly premiums and administrative fees from the
federal government and various states according to government specified payment rates and various contractual
terms. Changes in revenues from CMS for our Medicare products resulting from the periodic changes in risk-
adjustment scores for our membership are recognized when the amounts become determinable and the
collectibility is reasonably assured.
Medicare Part D Provisions
We cover prescription drug benefits in accordance with Medicare Part D under multiple contracts with
CMS. The payments we receive monthly from CMS and members, which are determined from our annual bid,
represent amounts for providing prescription drug insurance coverage. We recognize premium revenues for
providing this insurance coverage ratably over the term of our annual contract. Our CMS payment is subject to
risk sharing through the Medicare Part D risk corridor provisions. In addition, we receive and disburse amounts
for portions of prescription drug costs for which we are not at risk, as described more fully below.
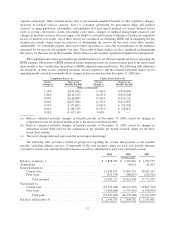
The risk corridor provisions compare costs targeted in our bids to actual prescription drug costs, limited to
actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding
certain thresholds may result in CMS making additional payments to us or require us to refund to CMS a portion
of the premiums we received. We estimate and recognize an adjustment to premium revenues related to these risk
corridor provisions based upon pharmacy claims experience to date as if the annual contract were to terminate at
the end of the reporting period. Accordingly, this estimate provides no consideration to future pharmacy claims
experience. We record a receivable or payable at the contract level and classify the amount as current or long-
term in the consolidated balance sheets based on the expected settlement.
The estimate of the settlement associated with risk corridor provisions requires us to consider factors that
may not be certain, including member eligibility differences with CMS. In 2009, we received net proceeds of
$59.6 million related to our reconciliation with CMS regarding the 2008 Medicare Part D risk corridor provisions
compared to our estimate of $55.4 million at December 31, 2008. In 2008, we paid $78.7 million related to our
reconciliation with CMS regarding the 2007 Medicare Part D risk corridor provisions compared to our estimate
of $102.6 million at December 31, 2007. The net liability associated with the 2009 risk corridor estimate, which
will be settled in 2010, was $144.6 million at December 31, 2009.
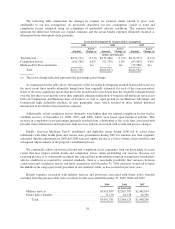
Reinsurance and low-income cost subsidies represent funding from CMS in connection with the Medicare
Part D program for which we assume no risk. Reinsurance subsidies represent funding from CMS for its portion
of prescription drug costs which exceed the member’s out-of-pocket threshold, or the catastrophic coverage level.
Low-income cost subsidies represent funding from CMS for all or a portion of the deductible, the coinsurance
and co-payment amounts above the out-of-pocket threshold for low-income beneficiaries. Monthly prospective
payments from CMS for reinsurance and low-income cost subsidies are based on assumptions submitted with our
annual bid. A reconciliation and related settlement of CMS’s prospective subsidies against actual prescription
drug costs we paid is made after the end of the year. We account for these subsidies as a deposit in our
consolidated balance sheets and as a financing activity in our consolidated statements of cash flows. We do not
recognize premium revenues or benefit expense for these subsidies. Receipt and payment activity is accumulated
at the contract level and recorded in our consolidated balance sheets in other current assets or trade accounts
60