Humana 2009 Annual Report Download - page 46
Download and view the complete annual report
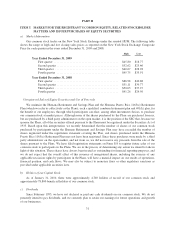
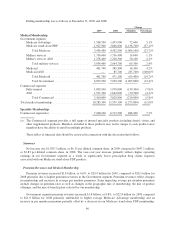
Please find page 46 of the 2009 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.experience in 2008, as well as an increase in the percentage of higher cost members. These issues were addressed
for 2009 based on enhancements made to our bid development and review processes. Our Medicare stand-alone
PDP membership declined to 1,927,900 members at December 31, 2009, down 1,138,700 members, or 37.1%,
from December 31, 2008, resulting primarily from our competitive positioning as we realigned stand-alone PDP
premium and benefit designs to correspond with our historical prescription drug claims experience. These actions
also resulted in a substantial decline in our stand-alone PDP benefit ratio for 2009 compared to 2008. We expect
Medicare stand-alone PDP membership to decrease by 50,000 to 100,000 members, or approximately 3% to 5%,
in 2010 as we continue to price and design benefits to correspond with our historical experience.
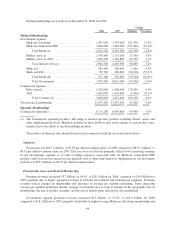
Our quarterly Government segment earnings and operating cash flows are impacted by the Medicare Part D
benefit design and changes in the composition of our membership. The Medicare Part D benefit design results in
coverage that varies as a member’s cumulative out-of-pocket costs pass through successive stages of a member’s
plan period which begins annually on January 1 for renewals. These plan designs generally result in us sharing a
greater portion of the responsibility for total prescription drug costs in the early stages and less in the latter
stages. As a result, the Government segment’s benefit ratio generally improves as the year progresses. In
addition, the number of low-income senior members as well as year-over-year changes in the mix of membership
in our stand-alone PDP products affect the quarterly benefit ratio pattern.
Our military services business primarily consists of the TRICARE South Region contract which covers
benefits for healthcare services provided to beneficiaries through March 31, 2010. On December 16, 2009, we
were notified by Department of Defense TRICARE Management Activity, or TMA, that it intends to exercise its
options to extend the TRICARE South Region contract for Option Period VII and Option Period VIII. The
exercise of these option periods would effectively extend the TRICARE South Region contract through
March 31, 2011. In July 2009, we were notified by the Department of Defense that we were not awarded the third
generation TRICARE program contract for the South Region which had been subject to competing bids. We filed
a protest with the Government Accountability Office, or GAO, in connection with the award to another
contractor citing discrepancies between the award criteria and procedures prescribed in the request for proposals
issued by the DoD and those that appear to have been used by the DoD in making its contractor selection. In
October 2009, we learned that the GAO had upheld our protest, determining that the TMA evaluation of our
proposal had unreasonably failed to fully recognize and reasonably account for the likely cost savings associated
with our record of obtaining network provider discounts from our established network in the South Region. On
December 22, 2009, we were advised that TMA notified the GAO of its intent to implement corrective action
consistent with the discussion contained within the GAO’s decision with respect to our protest. At this time, we
are not able to determine what actions TMA will take in response to recommendations by the GAO, nor can we
determine whether or not the protest decision by the GAO will have any effect upon the ultimate disposition of
the contract award. For 2009, premiums and ASO fees associated with the TRICARE South Region contract
were $3.4 billion, or 11.2% of our total premiums and ASO fees. We are continuing to evaluate issues associated
with our military services businesses such as potential impairment of certain assets primarily consisting of
goodwill, which had a carrying value of $49.8 million at December 31, 2009, potential exit costs, possible asset
sales, and a strategic assessment of ancillary businesses. Goodwill was not impaired at December 31, 2009.
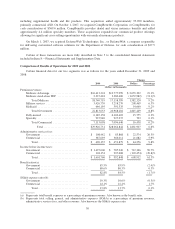
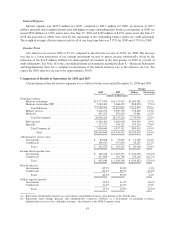
Commercial Segment
Commercial segment pretax earnings, impacted by the economic recession and the highly competitive
environment partially offset by higher investment income, decreased by $103.5 million, or 49.8%, for 2009
compared to 2008. Commercial segment medical membership at December 31, 2009 of 3,410,800 decreased
210,000 members, or 5.8% from December 31, 2008. The decline in membership primarily was a result of the
impact of the economic recession, including the loss of two larger ASO accounts. The economic recession has
led to increased in-group member attrition as employers reduce their workforce levels primarily through
reductions of less experienced workers. As a result, we experienced higher utilization of benefits, mainly in our
fully-insured group accounts, primarily due to the shift in the mix of members to an older workforce having more
health care needs, as well as members utilizing more benefits ahead of actual or perceived layoffs, members
36