Humana 2009 Annual Report Download - page 17
Download and view the complete annual report
Please find page 17 of the 2009 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.receive a fixed monthly payment from a government agency for which we are required to provide health
insurance coverage to enrolled members. Due to the increased emphasis on state health care reform and
budgetary constraints, more states are utilizing a managed care product in their Medicaid programs.
Our Medicaid business, which accounted for premium revenues of approximately $646.2 million, or 2.1%,
of our total premiums and ASO fees for the year ended December 31, 2009, consists of contracts in Puerto Rico
and Florida, with the vast majority in Puerto Rico.
Military Services
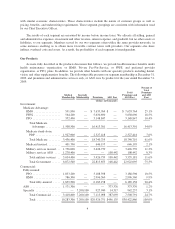
Under our TRICARE South Region contract with the United States Department of Defense, or DoD, we
provide health insurance coverage to the dependents of active duty military personnel and to retired military
personnel and their dependents. Currently, three health benefit options are available to TRICARE beneficiaries.
In addition to a traditional indemnity option, participants may enroll in a HMO-like plan with a point-of-service
option or take advantage of reduced copayments by using a network of preferred providers, similar to a PPO.
We have participated in the TRICARE program since 1996 under contracts with the Department of Defense.
Our current TRICARE South Region contract, which we were awarded in 2003, covers approximately
3.0 million eligible beneficiaries as of December 31, 2009 in Florida, Georgia, South Carolina, Mississippi,
Alabama, Tennessee, Louisiana, Arkansas, Texas and Oklahoma. The South Region is one of the three regions in
the United States as defined by the Department of Defense. Of these eligible beneficiaries, 1.3 million were
TRICARE ASO members representing active duty beneficiaries, seniors over the age of 65 and beneficiaries in
Puerto Rico for which the Department of Defense retains all of the risk of financing the cost of their health
benefit. We have subcontracted with third parties to provide selected administration and specialty services under
the contract. The original 5-year South Region contract expired March 31, 2009. Through an Amendment of
Solicitation/Modification of Contract to the TRICARE South Region contract, an additional one-year option
period, the sixth option period, which runs from April 1, 2009 through March 31, 2010, was exercised by the
government. The Amendment also provides for two additional six-month option periods: the seventh option
period runs from April 1, 2010 through September 30, 2010 and the eighth option period runs from October 1,
2010 through March 31, 2011. Exercise of each of the seventh and eighth option periods is at the government’s
option. On December 16, 2009, we were notified by Department of Defense TRICARE Management Activity, or
TMA, that it intends to exercise its options to extend the TRICARE South Region contract for Option Period VII
and Option Period VIII. The exercise of these option periods would effectively extend the TRICARE South
Region contract through March 31, 2011. The contract’s transition provisions require the continuation of certain
activities, primarily claims processing, during a wind-down period lasting approximately six months following
the expiration date. Claims incurred on or prior to the expiration date would continue to be processed during the
wind-down period under the terms existing prior to the expiration date.
The TRICARE South Region contract contains provisions that require us to negotiate a target health care
cost amount annually with the federal government. Any variance from the target health care cost is shared with
the federal government. Accordingly, events and circumstances not contemplated in the negotiated target health
care cost amount may have a material adverse effect on us. These changes may include an increase or reduction
in the number of persons enrolled or eligible to enroll due to the federal government’s decision to increase or
decrease U.S. military deployments.
In July 2009, we were notified by the Department of Defense that we were not awarded the third generation
TRICARE program contract for the South Region which had been subject to competing bids. We filed a protest
with the Government Accountability Office, or GAO, in connection with the award to another contractor citing
discrepancies between the award criteria and procedures prescribed in the request for proposals issued by the
DoD and those that appear to have been used by the DoD in making its contractor selection. In October 2009, we
learned that the GAO had upheld our protest, determining that the TMA evaluation of our proposal had
unreasonably failed to fully recognize and reasonably account for the likely cost savings associated with our
7