Humana 2004 Annual Report Download
Download and view the complete annual report
Please find the complete 2004 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Table of contents
-
Page 1
฀ ฀ -
Page 2
฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ -
Page 3
฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ... -
Page 4
... total฀ solutions฀ that฀ reduce฀ health฀ care฀ costs฀ while฀ offering฀ employers฀ and฀ employees฀ a฀ superior฀ health฀plan฀experience.฀We฀believe฀we฀have฀a฀signiï¬cant฀market฀advantage฀in฀both฀Medicare฀and฀innovative฀ commercial฀products... -
Page 5
...problems฀ in฀health฀insurance฀increasingly฀lining฀up฀with฀our฀internal฀vision.฀First฀and฀foremost,฀rising฀health฀care฀costs฀ have฀taken฀center฀stage฀as฀one฀of฀the฀crucial฀issues฀for฀businesses฀and฀individuals฀in฀the฀United฀States... -
Page 6
...include฀traditional฀HMOs฀and฀PPOs฀as฀well฀as฀ consumer-choice฀plans.฀These฀options฀are฀surrounded฀by฀Internet-based฀guidance฀tools฀that฀transform฀passive฀ health-care฀users฀into฀savvy,฀value-conscious฀health-care฀consumers.฀Through฀actionable... -
Page 7
...฀products,฀ including฀our฀ new฀SmartExpress฀offering฀for฀ groups฀of฀ 2฀ to฀299฀ employees.฀Although฀it's฀too฀ early฀to฀ be฀ certain,฀we฀think฀we're฀seeing฀the฀beginnings฀of฀a฀return฀to฀rational฀pricing฀in฀our฀commercial฀markets... -
Page 8
...฀ an฀ especially฀ large฀ opportunity฀ for฀ Humana,฀ both฀ in฀ terms฀ of฀ expanding฀our฀local฀Medicare฀PPOs฀and฀participating฀in฀regional฀PPOs฀in฀2006฀and฀beyond.฀ ฀ Commercial฀portfolio฀migration In฀the฀commercial฀business,฀the฀key... -
Page 9
...฀spending฀accounts฀and฀health฀reimbursement฀accounts. When฀you฀evaluate฀Humana฀for฀the฀longer฀term,฀these฀are฀some฀of฀the฀aspects฀you'll฀ continue฀to฀see A฀consumer฀company฀slowing฀the฀growth฀of฀health฀care฀costs฀and฀providing... -
Page 10
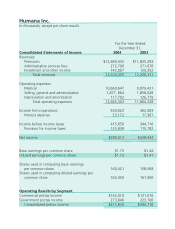
...,฀except฀per฀share฀results Consolidated฀Statements฀of฀Income฀ ฀ Revenues:฀ ฀ Premiums Administrative฀services฀fees Investment฀and฀other฀income฀ ฀ ฀ Total฀revenues฀ ฀ Operating฀expenses:฀ ฀ Medical฀ ฀ Selling,฀general฀and฀administrative... -
Page 11
... as specified in its charter) HUMANA INC. Delaware (State of incorporation) 61-0647538 (I.R.S. Employer Identification Number) 500 West Main Street Louisville, Kentucky (Address of principal executive offices) 40202 (Zip Code) Registrant's telephone number, including area code: (502) 580-1000... -
Page 12
...Item 14. Item 15. Part I Business Properties Legal Proceedings Submission of Matters to a Vote of Security Holders Part II Market for the Registrant's Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities Selected Financial Data Management's Discussion and Analysis of... -
Page 13
...premiums and administrative services fees in 2004 were earned from contracts with employer groups and individuals covering members located in Texas, Illinois, Florida, Kentucky and Ohio. We were organized as a Delaware corporation in 1964. Our principal executive offices are located at 500 West Main... -
Page 14
...Fees Medical Membership Specialty Membership Total Premiums and Premiums ASO Fees ASO Fees (dollars in thousands) Commercial: Fully insured: HMO ...PPO ...Total fully insured ...Administrative services only ...Specialty ...Total Commercial ...Government: Medicare Advantage ...Medicaid ...TRICARE... -
Page 15
... must approve access to many of these other health care providers, the HMO product is considered the most restrictive form of a health benefit plan. An HMO member, typically through the member's employer, pays a monthly fee, which generally covers, together with some copayments, health care services... -
Page 16
... traditional Medicare are still required to pay out-of-pocket deductibles and coinsurance. We contract with the Centers for Medicare and Medicaid Services, or CMS, under the Medicare Advantage program to provide health insurance benefits to Medicare eligible persons under HMO, PPO and Private Fee... -
Page 17
...operated to facilitate the delivery of health care services to lowincome residents. Each electing state develops, through a state specific regulatory agency, a Medicaid managed care initiative that must be approved by CMS. CMS requires that Medicaid managed care plans meet federal standards and cost... -
Page 18
... a fixed monthly payment from a government agency for which we are required to provide health insurance coverage to enrolled members. Due to the increased emphasis on state health care reform and budgetary constraints, more states are utilizing a managed care product in their Medicaid programs. We... -
Page 19
... summarizes our total medical membership at December 31, 2004, by market and product: Commercial HMO PPO ASO Government Medicare Advantage Medicaid TRICARE (in thousands) Percent of Total Total Florida ...Texas ...Illinois ...Puerto Rico ...Kentucky ...Ohio ...Wisconsin ...Louisiana ...Arizona... -
Page 20
...in our HMO networks are reimbursed based upon a fixed fee schedule, which typically provides for reimbursement based upon a percentage of the standard Medicare allowable fee schedule. Capitation For 5.3% of our December 31, 2004 medical membership, we contract with hospitals and physicians to accept... -
Page 21
... Fully Total Insured ASO Segment Medical Membership: December 31, 2004 Capitated HMO hospital system based ...70,300 Capitated HMO physician group based ...56,300 Risk-sharing ...68,000 Other ...2,091,900 Total ...2,286,500 Medicare Advantage Government Segment TRICARE Medicaid TRICARE ASO Total... -
Page 22
... operations providing personal nurse services, pharmacy management, and disease management. Sales and Marketing Individuals become members of our commercial HMOs and PPOs through their employers or other groups which typically offer employees or members a selection of health insurance products, pay... -
Page 23
... resources than our health plans in the markets in which we compete. Our ability to sell our products and to retain customers is, or may be, influenced by such factors as benefits, pricing, contract terms, number and quality of participating physicians and other providers, utilization review, claims... -
Page 24
..., Humana Insurance Company holds CMS contracts under a Medicare Advantage program to sell a private fee-for-service product in eleven states and PPO plans in many of our existing markets. The PPO and HMO plans are considered "coordinated care plans" and have similar standards. CMS conducts audits... -
Page 25
... under state insurance holding company and Commonwealth of Puerto Rico regulations. These regulations generally require, among other things, prior approval and/or notice of new products, rates, benefit changes, and certain material transactions, including dividend payments, purchases or sales... -
Page 26
.... Mandate-free benefit plans are pending in a number of states. Some of these proposals could allow insurers more flexibility in the use of member cost sharing. There is activity in some states supporting an expansion of disclosure by hospitals, physicians, and other health care providers of quality... -
Page 27
...located in the Humana Building, 500 West Main Street, Louisville, Kentucky 40202. In addition, as of December 31, 2004, we own buildings in Louisville, Kentucky, and Green Bay, Wisconsin, and lease facilities in Cincinnati, Ohio and Puerto Rico, all of which are used for customer service, enrollment... -
Page 28
... provider operators. The following table lists the location of properties we owned or leased at December 31, 2004: Medical Centers Owned Leased Administrative Offices Owned Leased Total Florida ...Texas ...Kentucky ...Georgia ...Illinois ...Puerto Rico ...Louisiana ...Tennessee ...Alabama ...Ohio... -
Page 29
... federal regulatory authorities. There has been increased scrutiny by these regulators of the managed health care companies' business practices, including allegations of anticompetitive and unfair business activities, claims payment practices, commission payment practices, and utilization management... -
Page 30
...certain software products in processing claims. Pending state and federal legislative activity may increase our exposure for any of these types of claims. In addition, some courts have issued rulings which make it easier to hold plans liable for medical negligence on the part of network providers on... -
Page 31
... 12 of the Exchange Act: Total Number of Shares Purchased (1) Average Price Paid per Share Total Number of Shares Purchased as Part of Publicly Announced Plans or Programs (2)(3) Dollar Value of Shares that May Yet Be Purchased Under the Plans or Programs (2) Period January 2004 ...February 2004... -
Page 32
... pay dividends, and we currently plan to retain our earnings for future operations and growth of our businesses. e) Equity Compensation Plan The information required by this part of Item 5 is incorporated herein by reference from our Proxy Statement for the Annual Meeting of Stockholders scheduled... -
Page 33
......Medical Membership by Segment Commercial: Fully insured ...Administrative services only ...Total Commercial ...Government: Medicare Advantage ...Medicaid ...TRICARE ...TRICARE ASO ...Total Government ...Total Medical Membership ...Commercial Specialty Membership Dental ...Other ...Total specialty... -
Page 34
...with the Centers for Medicare and Medicaid Services, or CMS. Additionally, 37% of our premiums and administrative services fees in 2004 were earned from contracts with employer groups and individuals covering members located in Texas, Illinois, Florida, Kentucky and Ohio. We manage our business with... -
Page 35
... only through our consumer-choice products, but also by (1) expanding our ASO membership to take advantage of our network discounts in the mid-market group segment and (2) launching our HumanaOne individual product to address an increasing migration of insureds from small group. While we expect our... -
Page 36
...-Service plans in eleven new states, and recently have received approvals from CMS establishing Local Medicare PPO plans in many of our existing markets where we have established competitive networks. Medicare Private Fee-ForService plans generally offer additional benefits compared to traditional... -
Page 37
... in cash. Ochsner, a Louisiana health plan, added approximately 152,600 commercial medical members, primarily in fully insured large group accounts, and approximately 33,100 members in the Medicare Advantage program. This acquisition enabled us to enter a new market with significant market share... -
Page 38
... ratios) Premium revenues: Fully insured ...Specialty ...Total Commercial ...Medicare Advantage ...TRICARE ...Medicaid ...Total Government ...Total ...Administrative services fees: Commercial ...Government ...Total ...Income before income taxes: Commercial ...Government ...Total ...Medical expense... -
Page 39
... totaling approximately 94,000 members in 2004 and continued attrition due to the ongoing competitive environment within the small to mid-market group fullyinsured accounts, partially offset by membership gains in the Individual product lines. We expect fully insured commercial per member premiums... -
Page 40
... from the transition to the new South Region contract which carved out certain government programs including the administration of pharmacy and medical benefits to senior members over the age of 65. We stopped providing services under these separate programs beginning June 1, 2004. Investment and... -
Page 41
... depreciation from reducing the estimated useful life of software increased depreciation expense $9.3 million in 2004 and $13.5 million in 2003. We review the carrying value and useful life of software when changes in the use of the asset in our operations indicate the carrying value may not... -
Page 42
...) Premium revenues: Fully insured ...Specialty ...Total Commercial ...Medicare Advantage ...TRICARE ...Medicaid ...Total Government ...Total ...Administrative services fees: Commercial ...Government ...Total ...Income (loss) before income taxes: Commercial ...Government ...Total ...Medical expense... -
Page 43
... counties in some of our markets effective January 1, 2003 and general attrition in certain markets as a result of annual changes to benefit designs. Per member Medicare premiums increased in the 4% to 6% range for 2003. Administrative Services Fees Administrative services fees for 2003 were $271... -
Page 44
... $14.8 million. Increased operating efficiency led to the consolidation of seven service centers into four and an enterprisewide workforce reduction affecting administrative expenses in both 2003 and 2002 by recording expenses for severance and related employee benefit costs and building impairments... -
Page 45
...or one business day later. Therefore, we received only 11 monthly Medicare Advantage premium remittances during 2004 versus 12 monthly premium remittances during 2003. Other than the impact from the timing of the Medicare Advantage premium receipts, the increase in net income and cash generated from... -
Page 46
... the new TRICARE South region contract, the fixed price and BPA process was eliminated and replaced with a new reimbursement model. Under the new reimbursement model, claims paid are reimbursed by the federal government generally within 30 business days. The delivery of health care services results... -
Page 47
...service centers in Jacksonville and San Antonio including the sale of the Jacksonville office tower in 2004 for $14.8 million and a San Antonio office building for $5.9 million in 2003. Cash Flow from Financing Activities We repurchased 3.8 million common shares for $67.0 million at an average price... -
Page 48
...most states, prior notification is provided before paying a dividend even if approval is not required. As of December 31, 2004, we maintained aggregate statutory capital and surplus of $1,185.5 million in our state regulated health insurance subsidiaries. Each of these subsidiaries was in compliance... -
Page 49
...Through indemnity agreements approved by the state regulatory authorities, certain of our regulated subsidiaries generally are guaranteed by Humana Inc., our parent company, in the event of insolvency for (1), member coverage for which premium payment has been made prior to insolvency; (2), benefits... -
Page 50
... $ 10,144 Our HMO, PPO and Fee-For-Service products covered under the Medicare Advantage contracts with the federal government are renewed for a one-year term each December 31 unless notice of termination is received at least 90 days prior thereto. No termination notices were received in connection... -
Page 51
...2004, Puerto Rico accounted for approximately 83% of our total Medicaid membership. The loss of any of the contracts above or significant changes in these programs as a result of legislative action, including reductions in premium payments to us, or increases in member benefits without corresponding... -
Page 52
... cost trends include increases in the utilization of hospital facilities, physician services, prescription drugs, and new medical technologies, as well as the inflationary effect on the cost per unit of each of these expense components. Other external factors such as government-mandated benefits... -
Page 53
... percentage of our Medicare and Medicaid membership under risk-sharing arrangements with providers. Accordingly, the impact of changes in estimates for prior year medical claims payable on our results from operations that are attributable to our Medicare and Medicaid lines of business may also be... -
Page 54
... estimated utilization of medical services by TRICARE beneficiaries in the second half of 2002. Revenue Recognition We generally establish one-year contracts with commercial employer groups, subject to cancellation by the employer group's 30-day written notice. Our contracts with federal or state... -
Page 55
...reimbursed by the federal government; and, (3) administrative service fees related to claim processing, customer service, enrollment, disease management and other services. We recognize the insurance premium as revenue ratably over the period coverage is provided. Health care services reimbursements... -
Page 56
... quoted market price does not exist, are estimated using a variety of valuation methodologies. Such methodologies include reviewing the value ascribed to the most recent financing, comparing the security with securities of publicly traded companies in a similar line of business, and reviewing... -
Page 57
... of fully and self-insured medical and specialty. The Government segment's three reporting units consist of Medicare Advantage, TRICARE and Medicaid. Goodwill is assigned to the reporting unit that is expected to benefit from a specific acquisition. Our strategy, long-range business plan, and annual... -
Page 58
... issued Statement No. 123R, Share-Based Payment, or Statement 123R, which requires companies to expense the fair value of employee stock options and other forms of stock-based compensation. This requirement represents a significant change because fixed-based stock option awards, a predominate form... -
Page 59
... prescription drugs; increased cost of such services; the Company's membership mix; variances in actual versus estimated levels of cost associated with new products, benefits or lines of business, product changes or benefit level changes; membership in markets lacking adequate provider networks... -
Page 60
...or entrance to Medicare Advantage or Commercial markets. To determine the fixed monthly payments per member to pay to managed care plans, CMS has implemented a risk adjustment model that uses diagnosis data from ambulatory treatment settings (hospital outpatient department and physician visits). CMS... -
Page 61
..., have problems in determining medical cost estimates and establishing appropriate pricing, have customer and physician and other health care provider disputes, have regulatory problems, have increases in operating expenses, lose existing customers, have difficulty in attracting new customers, or... -
Page 62
...the TRICARE, Medicare Advantage, and Medicaid programs. These programs involve various risks, including: • At December 31, 2004, under one of our contracts with the Centers for Medicare and Medicaid Services, or CMS, we provided health insurance coverage to approximately 231,700 members in Florida... -
Page 63
..., results of operations and cash flows; • At December 31, 2004, our TRICARE business, which accounted for approximately 17% of our total premiums and ASO fees during 2004, consisted of the South Region contract. The South Region contract is a five-year contract, subject to annual renewals at the... -
Page 64
... mandatory benefits and products; rules tightening time periods in which claims must be paid; medical malpractice reform; defining medical necessity; health insurance access; provider compensation and contract language; disclosure of provider fee schedules and other data about payments to providers... -
Page 65
...deliver quality medical services in a cost-effective manner. In any particular market, providers could refuse to contract with us, demand to contract with us, demand higher payments, or take other actions that could result in higher health care costs for us, less desirable products for customers and... -
Page 66
... and administrative expense reimbursements from our subsidiaries to fund the obligations of Humana Inc., the parent company. These subsidiaries generally are regulated by states' Departments of Insurance. In most states, we are required to seek prior approval by these state regulatory authorities... -
Page 67
... cash equivalents ...Investment securities ...Receivables, less allowance for doubtful accounts of $34,506 in 2004 and $40,400 in 2003: Premiums ...Administrative services fees ...Securities lending collateral ...Other ...Total current assets ...Property and equipment, net ...Other assets: Long-term... -
Page 68
Humana Inc. CONSOLIDATED STATEMENTS OF INCOME For the year ended December 31, 2004 2003 2002 (in thousands, except per share results) Revenues: Premiums ...Administrative services fees ...Investment and other income ...Total revenues ...Operating expenses: Medical ...Selling, general and ... -
Page 69
... - - 10,785 - - 10,785 Common Stock Capital In Issued Excess of Shares Amount Par Value Comprehensive income ...Common stock repurchases ...Restricted stock forfeitures ...Restricted stock amortization ...Stock option exercises ...Stock option tax benefit ...Other stock compensation ...- (331) - 973... -
Page 70
...Debt issue costs ...Change in book overdraft ...Change in securities lending payable ...Common stock repurchases ...Proceeds from stock option exercises and other ...Net cash (used in) provided by financing activities ...(Decrease) increase in cash and cash equivalents ...Cash and cash equivalents... -
Page 71
... one federal government contract with the Centers for Medicare and Medicaid Services, or CMS, we provide health insurance coverage for Medicare Advantage members in Florida, accounting for approximately 15% of our total premiums and administrative services fees in 2004. We manage our business with... -
Page 72
... membership contracts with employer groups, subject to cancellation by a 30 day written notice. Our TRICARE contract with the federal government and our contracts with various state Medicaid programs generally are multi-year contracts subject to annual renewal provisions. Our Medicare Advantage... -
Page 73
...reimbursed by the federal government; and (3), administrative service fees related to claim processing, customer service, enrollment, disease management and other services. We recognize the insurance premium as revenue ratably over the period coverage is provided. Health care services reimbursements... -
Page 74
... our long-lived asset policy. Medical and Other Expenses Payable and Medical Cost Recognition Medical costs include claim payments, capitation payments, pharmacy costs net of rebates, allocations of certain centralized expenses and various other costs incurred to provide health insurance coverage to... -
Page 75
... medical care provided prior to the balance sheet date. Capitation payments represent monthly contractual fees disbursed to primary care physicians and other providers who are responsible for providing medical care to members. Pharmacy costs represent payments for members' prescription drug benefits... -
Page 76
... operating our Company such as professional and general liability, employee workers' compensation, and officer and director errors and omissions risks. Professional and general liability risks may include, for example, medical malpractice claims and disputes with members regarding benefit coverage... -
Page 77
... thousands, except per share results) Net income, as reported ...Add: Stock-based employee compensation expense included in reported net income, net of related tax ...Deduct: Total stock-based employee compensation expense determined under fair value based method for all awards, net of related tax... -
Page 78
... 10 medical centers and pharmacy company. CarePlus provides Medicare Advantage HMO plans and benefits to Medicare eligible members in Miami-Dade, Broward and Palm Beach counties. This acquisition enhances our Medicare market position in South Florida. We paid approximately $450 million in cash... -
Page 79
... and provider contracts, have a weighted-average useful life of approximately...cash purchase price and the associated income tax effects of the pro forma adjustments. The pro forma results have been prepared for comparative purposes only and do not purport to be indicative of the results of operations... -
Page 80
... states' insurance regulations. Gross unrealized losses and fair value aggregated by investment category and length of time that individual securities have been in a continuous unrealized loss position were as follows at December 31, 2004 and 2003: Less than 12 months 12 months or more Total... -
Page 81
... that a decline in fair value below the cost basis was other than temporary. We participate in a securities lending program where we loan certain investment securities for short periods of time in exchange for collateral, consisting of cash or U.S. Government securities, initially equal to at... -
Page 82
... accelerating depreciation related to abandoned software more fully described below. A decision to close the Jacksonville, Florida customer service center prompted a review for the possible impairment of long-lived assets associated with this center. Under a transition plan, we continued to use the... -
Page 83
...in thousands) Total Line item affected: Depreciation and amortization ...Total pretax impact ... $9,349 $9,349 $ $ - - $9,349 $9,349 Commercial 2003 Government (in thousands) Total Line item affected: Selling, general and administrative ...Depreciation and amortization ...Total pretax impact... -
Page 84
... estimated, representing 0.8% of medical claim expenses recorded in 2002. This $17.4 million change in the amounts incurred related to prior years resulted primarily from favorable development in our Medicare line of business as a result of better than expected utilization in the latter half of... -
Page 85
... percentage of our Medicare and Medicaid membership under risk-sharing arrangements with providers. Accordingly, the impact of changes in estimates for prior year medical claims payable on our results from operations that are attributable to our Medicare and Medicaid lines of business may also be... -
Page 86
... in the allowable carryforward period given our recent and historical capital gain experience and the consideration of alternative tax planning strategies. During 2002, the Internal Revenue Service completed their audit of all open years prior to 2000 which resulted in an adjustment to the estimated... -
Page 87
... short-term debt and take advantage of historically low interest rates, we issued $300 million 6.30% senior notes due August 1, 2018 on August 5, 2003. Our net proceeds, reduced for the cost of the offering, were approximately $295.8 million. The net proceeds were used for general corporate purposes... -
Page 88
... We maintain and may issue short-term debt securities under a commercial paper program when market conditions allow. The program is backed by our credit agreement described above. Aggregate borrowings under both the credit agreement and commercial paper program generally will not exceed $600 million... -
Page 89
... and general liability exposures. Since January 1, 2002, we have reduced the amount of coverage purchased from third party insurance carriers, causing an increase in the provision for professional liability risks and a decrease in the estimated recoverables from insurance. The total cost associated... -
Page 90
... the entire organization, including customer service, claim administration, clinical operations, provider network administration, as well as other corporate and field-based positions. We continually review estimates of future payments for probable severance benefits and make necessary adjustments to... -
Page 91
... 31, 2004, there were 15,543,781 shares reserved for employee and director stock option plans, including 5,451,095 shares of common stock available for future grants. On February 24, 2005, the Board of Directors approved the issuance of 2,595,700 additional options and restricted stock awards. 81 -
Page 92
... exercise price of $14.06. Compensation expense related to performance-based stock option awards, stock granted to directors and modifications to fixed-based stock option awards was $3.8 million in 2004, $0.5 million in 2003, and $0.5 million in 2002. The effects on net income and earnings per share... -
Page 93
... a share of Series A Participating Preferred Stock at a price of $145 per share. This plan expires in 2006. Regulatory Requirements Certain of our subsidiaries operate in states that regulate the payment of dividends, loans, or other cash transfers to Humana Inc., our parent company, require minimum... -
Page 94
... be in compliance and we would have $405.6 million of aggregate capital and surplus above any of the levels that require corrective action under RBC. 14. COMMITMENTS, GUARANTEES AND CONTINGENCIES Leases We lease facilities, computer hardware, and other equipment under long-term operating leases that... -
Page 95
... new opportunities in our Medicare programs, including our HMO, PPO, and Private Fee-For-Service products. We have made additional investments in the Medicare Advantage program to enhance our ability to participate in these expanded programs. Our TRICARE South Region contract, which we were awarded... -
Page 96
... fee-for-service class and five subclasses for the time period from January 1, 1996, to the date of certification. The global class would consist of any medical doctor who provided service on a fee-for-service basis to any person insured by Cigna Corporation or any other defendant for claims of RICO... -
Page 97
... federal regulatory authorities. There has been increased scrutiny by these regulators of the managed health care companies' business practices, including allegations of anticompetitive and unfair business activities, claims payment practices, commission payment practices, and utilization management... -
Page 98
..., and includes three lines of business: fully insured medical, administrative services only, or ASO, and specialty. The Government segment consists of members enrolled in government-sponsored programs, and includes three lines of business: Medicare Advantage, Medicaid, and TRICARE. We identified our... -
Page 99
...) 2002 Revenues: Premiums: Medicare Advantage ...TRICARE ...Medicaid ...Total premiums ...Administrative services fees ...Investment and other income ...Total revenues ...Operating expenses: Medical ...Selling, general and administrative ...Depreciation and amortization ...Total operating expenses... -
Page 100
... well-established, as evidenced by the strong financial ratings at December 31, 2004 presented below: Reinsurer Total Recoverable (in thousands) Rating (a) Protective Life Insurance Company ...All others ... $232,396 28,190 $260,586 A+ (superior) A to A- (excellent) (a) Ratings are published by... -
Page 101
... on these financial statements and financial statement schedules based on our audits. We conducted our audits of these statements in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain... -
Page 102
... in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (iii) provide reasonable assurance regarding prevention or timely detection of... -
Page 103
... Health Plan since April 1, 2004, the date of its acquisition. (b) Includes expenses of $30.8 million pretax ($18.8 million after tax, or $0.12 per diluted share) for the writedown of building and equipment and software abandonment expenses due to the elimination of three customer service centers... -
Page 104
... in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (iii) provide reasonable assurance regarding prevention or timely detection of... -
Page 105
..., LLP, our independent registered public accounting firm who also audited the Company's consolidated financial statements included in our Annual Report on Form 10-K, as stated in their report which appears on page 91. Michael B. McCallister President and Chief Executive Officer James H. Bloem Senior... -
Page 106
...-Chief Financial Officer and Treasurer Senior Vice President-Chief Service and Information Officer Senior Vice President-Chief Human Resources Officer Senior Vice President-General Counsel Senior Vice President-Strategy and Corporate Development Senior Vice President-Chief Innovation Officer... -
Page 107
...-Government Programs (TRICARE) and Puerto Rico having held this position since February 2001 and is retiring effective March 31, 2005. Mr. Shields previously served as Senior Vice President-Development from February 2001 to June 2001 and Senior Vice President and Chief Operating Officer-Emphesys... -
Page 108
.... All employees and directors are required to annually affirm in writing their acceptance of the code. The Humana Inc. Principles of Business Ethics was adopted by our Board of Directors in February 2004 as the document to comply with the New York Stock Exchange Corporate Governance Standard 303A.10... -
Page 109
...required by Sections 302 and 906 of the Sarbanes-Oxley Act. These certifications are filed as Exhibits to this Annual Report on Form 10-K. Additionally, our CEO has signed the December 31, 2003 certificate as to compliance with the Corporate Governance Listing Standards adopted by the New York Stock... -
Page 110
... "Audit Committee Report" of such Proxy Statement. Audit Committee Pre-approval Policies and Procedures The information required by this Item is herein incorporated by reference from our Proxy Statement for the Annual Meeting of Stockholders scheduled to be held on April 26, 2005 appearing under the... -
Page 111
... to the 1989 Stock Option Plan for Employees. Annex B to the Company's Proxy Statement covering the Annual Meeting of Stockholders held on February 18, 1993, is incorporated by reference herein. 101 Parent Company Financial Information Valuation and Qualifying Accounts All other schedules have been... -
Page 112
... herein. Humana Inc. Non-Qualified Stock Option Plan for Employees. Exhibit 99 to the Company's Form S-8 Registration Statement (333-86801) filed on September 9, 1999, is incorporated by reference herein. Form of Company's Stock Option Agreement under the 1996 Stock Incentive Plan for Employees (Non... -
Page 113
... 1996 Stock Incentive Plan, filed herewith. (dd)* Form of Company's Restricted Stock Agreement under the 2003 Stock Incentive Plan, filed herewith. (ee) Agreement between the Secretary of the Department of Health and Human Services and Humana Medical Plan, Inc. Exhibit 10(w) to the Company's Annual... -
Page 114
14 Code of Conduct for Chief Executive Officer & Senior Financial Officers. Exhibit 14 to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 2003, is incorporated by reference herein. List of subsidiaries, filed herewith. Consent of PricewaterhouseCoopers LLP, filed ... -
Page 115
Humana Inc. SCHEDULE I-PARENT COMPANY FINANCIAL INFORMATION CONDENSED BALANCE SHEETS December 31, 2004 2003 (in thousands, except share amounts) ASSETS Current assets: Cash and cash equivalents ...Investment securities ...Receivable from operating subsidiaries ...Securities lending collateral ...... -
Page 116
Humana Inc. SCHEDULE I-PARENT COMPANY FINANCIAL INFORMATION CONDENSED STATEMENTS OF OPERATIONS For the year ended December 31, 2004 2003 2002 (in thousands) Revenues: Management fees charged to operating subsidiaries ...Investment income (loss) and other income, net ...Expenses: Selling, general ... -
Page 117
Humana Inc. SCHEDULE I-PARENT COMPANY FINANCIAL INFORMATION CONDENSED STATEMENTS OF CASH FLOWS For the year ended December 31, 2004 2003 (in thousands) 2002 Net cash provided by operating activities ...Cash flows from investing activities: Purchases of investment securities ...Proceeds from sale of... -
Page 118
... agreements approved, if required, by state regulatory authorities, Humana Inc., our parent company, charges a management fee for reimbursement of certain centralized services provided to its subsidiaries including information systems, disbursement, investment and cash administration, marketing... -
Page 119
Humana Inc. SCHEDULE II-VALUATION AND QUALIFYING ACCOUNTS For the Years Ended December 31, 2004, 2003, and 2002 (in thousands) Additions Charged (Credited) to Charged to Costs and Other Expenses Accounts (1) Balance at Beginning of Period Acquired Balances Deductions or Write-offs Balance at End... -
Page 120
... duly authorized. HUMANA INC. By: /s/ JAMES H. BLOEM James H. Bloem Senior Vice President and Chief Financial Officer Date:March 1, 2005 Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the Company and... -
Page 121
-
Page 122
฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀ ฀... -
Page 123
Corporate฀Headquarters The฀Humana฀Building 500฀West฀Main฀Street Louisville,฀Kentucky฀฀40202 (502)฀580-1000 More฀Information฀About฀Humana฀Inc. Copies฀of฀the฀Company's฀ï¬lings฀with฀the฀Securities฀and฀Exchange฀Commission฀may฀be฀obtained฀without... -
Page 124