Humana 2004 Annual Report Download - page 16
Download and view the complete annual report
Please find page 16 of the 2004 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Specialty Products
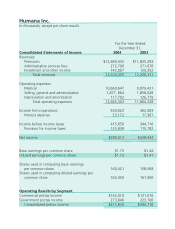
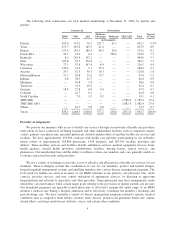
We additionally offer various specialty products including dental, group and individual life, and short-term
disability. At December 31, 2004, we had approximately 1.7 million specialty members, including 1.2 million
dental members. For the year ended December 31, 2004, specialty product premium revenues were
approximately $349.6 million, or 2.7% of our total premiums and ASO fees.
Our Products Marketed to Government Segment Members and Beneficiaries
Medicare Advantage Products
Medicare is a federal program that provides persons age 65 and over and some disabled persons under the
age of 65 certain hospital and medical insurance benefits. Hospitalization benefits are provided under Part A,
without the payment of any premium, for up to 90 days per incident of illness plus a lifetime reserve aggregating
60 days. Eligible beneficiaries are required to pay an annually adjusted premium to the federal government to be
eligible for physician care and other services under Part B. Beneficiaries eligible for Part A and Part B coverage
under traditional Medicare are still required to pay out-of-pocket deductibles and coinsurance.
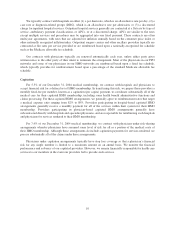
We contract with the Centers for Medicare and Medicaid Services, or CMS, under the Medicare Advantage
program to provide health insurance benefits to Medicare eligible persons under HMO, PPO and Private Fee-For-
Service, or PFFS, plans in exchange for contractual payments received from CMS. With each of these products
the beneficiary generally receives benefits in excess of traditional Medicare, typically including a prescription
drug benefit, a reduced monthly premium, or reduced cost sharing. Medicare Advantage plans may charge
beneficiaries monthly premiums and other copayments for Medicare-covered services or for certain extra
benefits. Beginning in 2006, Medicare beneficiaries will have a prescription drug benefit, and most Medicare
Advantage plans must offer that benefit as part of the basic plan.
For our Medicare HMO and PPO plans, we contract with CMS to provide health insurance benefits in
exchange for a fixed monthly payment per member for Medicare-eligible individuals residing in defined
counties. Individuals who elect to participate in these plans receive benefits in excess of traditional Medicare.
These benefits typically include a prescription drug benefit, subject to cost sharing and some limitations.
Additionally, these benefits may eliminate or reduce coinsurance or the level of deductibles on many other
medical services while seeking care from participating in-network providers, or in emergency situations. Except
in emergency situations, HMO plans provide no out-of-network benefits. PPO plans carry an out-of network
benefit that is subject to higher member cost-sharing. In many cases, these beneficiaries also may be required to
pay a monthly premium to the HMO or PPO plan, in addition to the monthly Part B premium they are required to
pay the Medicare program.
For our Medicare PFFS plans, we contract with CMS to offer health benefits to eligible Medicare
beneficiaries in certain states in exchange for a fixed monthly payment per member. Under these plans, we offer
a prescription drug benefit, subject to cost sharing and other limitations. Other health care benefits also may be
different than traditional Medicare. Individuals in these plans pay a monthly premium to receive these enhanced
prescription drug benefits. Unlike the HMO and PPO plans, these plans have no preferred network.
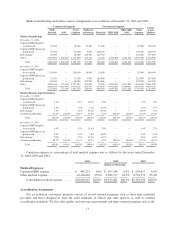
Medicare uses monthly rates per person for each county to determine the fixed monthly payments per
member to pay to managed care plans. In the last decade, Congress has made several changes to how CMS must
calculate these rates. The old (pre-1998) methodology was based on the Adjusted Average Per Capita Cost
methodology, or AAPCC. Under AAPCC, CMS projected average county-level fee-for-service spending for the
coming year to set the reimbursement rates for Medicare health plans at 95 percent of the full AAPCC amount.
Under the AAPCC system, payment rates per county varied widely. For example, the 1997 capitation rate
for beneficiaries 65 and older for Part A and Part B services ranged from a low of $220.92 in Arthur County,
Nebraska to a high of $767.35 in Richmond County, Staten Island, New York. Some states saw differences of
more than 20 percent between adjacent counties. Since county fee-for-service costs were used to estimate county
managed care capitation rates, the rates reflected differences among counties and regions in fee-for-service
utilization patterns and cost structures.
6