Humana 2004 Annual Report Download - page 20
Download and view the complete annual report
Please find page 20 of the 2004 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.We typically contract with hospitals on either (1) a per diem rate, which is an all-inclusive rate per day, (2) a
case rate or diagnosis-related groups (DRG), which is an all-inclusive rate per admission, or (3) a discounted
charge for inpatient hospital services. Outpatient hospital services generally are contracted at a flat rate by type of
service, ambulatory payment classifications, or APCs, or at a discounted charge. APCs are similar to flat rates
except multiple services and procedures may be aggregated into one fixed payment. These contracts are often
multi-year agreements, with rates that are adjusted for inflation annually based on the consumer price index or
other nationally recognized inflation index. Outpatient surgery centers and other ancillary providers typically are
contracted at flat rates per service provided or are reimbursed based upon a nationally-recognized fee schedule
such as the Medicare allowable fee schedule.
Our contracts with physicians typically are renewed automatically each year, unless either party gives
written notice to the other party of their intent to terminate the arrangement. Most of the physicians in our PPO
networks and some of our physicians in our HMO networks are reimbursed based upon a fixed fee schedule,
which typically provides for reimbursement based upon a percentage of the standard Medicare allowable fee
schedule.
Capitation
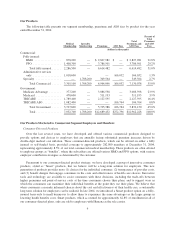
For 5.3% of our December 31, 2004 medical membership, we contract with hospitals and physicians to
accept financial risk for a defined set of HMO membership. In transferring this risk, we prepay these providers a
monthly fixed-fee per member, known as a capitation (per capita) payment, to coordinate substantially all of the
medical care for their capitated HMO membership, including some health benefit administrative functions and
claims processing. For these capitated HMO arrangements, we generally agree to reimbursement rates that target
a medical expense ratio ranging from 82% to 89%. Providers participating in hospital-based capitated HMO
arrangements generally receive a monthly payment for all of the services within their system for their HMO
membership. Providers participating in physician-based capitated HMO arrangements generally have
subcontracted directly with hospitals and specialist physicians, and are responsible for reimbursing such hospitals
and physicians for services rendered to their HMO membership.
For 7.4% of our December 31, 2004 medical membership, we contract with physicians under risk-sharing
arrangements whereby physicians have assumed some level of risk for all or a portion of the medical costs of
their HMO membership. Although these arrangements do include capitation payments for services rendered, we
process substantially all of the claims under these arrangements.
Physicians under capitation arrangements typically have stop loss coverage so that a physician’s financial
risk for any single member is limited to a maximum amount on an annual basis. We monitor the financial
performance and solvency of our capitated providers. However, we remain financially responsible for health care
services to our members in the event our providers fail to provide such services.
10