Humana 2004 Annual Report Download - page 52
Download and view the complete annual report
Please find page 52 of the 2004 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
estimate of our medical and other expenses payable at December 31, 2004, which represents approximately 40%
of total liabilities, would require an adjustment of approximately $14 million in a future period in which a
revision in the estimate became known.
We develop our estimate for IBNR using actuarial methodologies and assumptions, primarily based upon
historical claim payment and claim receipt patterns, as well as historical medical cost trends. Depending on the
period for which incurred claims are estimated, we apply a different method in determining our estimate. For
periods prior to the most recent three months, the key assumption used in estimating our IBNR is that the
completion factor pattern remains consistent over a rolling 12-month period after adjusting for known changes in
claim inventory levels and known changes in claim payment processes. Completion factors result from the
calculation of the percentage of claims incurred during a given period that have historically been adjudicated as
of the reporting period. For the most recent three months, the incurred claims are estimated primarily from a
trend analysis based upon per member per month claims trends developed from our historical experience in the
preceding months, adjusted for known changes in estimates of recent hospital and drug utilization data, provider
contracting changes, changes in benefit levels, product mix, and weekday seasonality.
The completion factor method is used for the months of incurred claims prior to the most recent three
months because the historical percentage of claims processed for those months is at a level sufficient to produce a
consistently reliable result. Conversely, for the most recent three months of incurred claims, the volume of claims
processed historically is not at a level sufficient to produce a reliable result, which therefore requires us to
examine historical trend patterns as the primary method of evaluation.
Medical cost trends potentially are more volatile than other segments of the economy. The drivers of
medical cost trends include increases in the utilization of hospital facilities, physician services, prescription
drugs, and new medical technologies, as well as the inflationary effect on the cost per unit of each of these
expense components. Other external factors such as government-mandated benefits or other regulatory changes,
increases in medical services capacity, direct to consumer advertising for prescription drugs and medical
services, an aging population, catastrophes, and epidemics also may impact medical cost trends. Internal factors
such as system conversions, claims processing cycle times, changes in medical management practices and
changes in provider contracts also may impact our ability to accurately predict estimates of historical completion
factors or medical cost trends. All of these factors are considered in estimating IBNR and in estimating the per
member per month claims trend for purposes of determining the reserve for the most recent three months.
Additionally, we continually prepare and review follow-up studies to assess the reasonableness of the estimates
generated by our process and methods over time. The results of these studies are also considered in determining
the reserve for the most recent three months. Each of these factors requires significant judgment by management.
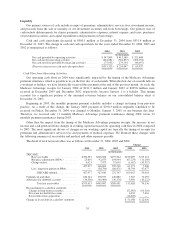
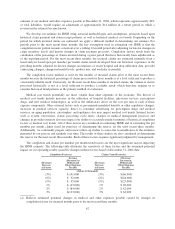
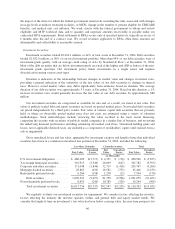
The completion and claims per member per month trend factors are the most significant factors impacting
the IBNR estimate. The following table illustrates the sensitivity of these factors and the estimated potential
impact on our operating results caused by changes in these factors based on December 31, 2004 data:
Completion Factor(a): Claims Trend Factor(b):
(Decrease)
Increase
in Factor
Increase
(Decrease) in
Medical and
Other Expenses
Payable
(Decrease)
Increase
in Factor
(Decrease)
Increase in
Medical and
Other Expenses
Payable
(dollars in thousands)
(3%) $ 141,000 (3%) $(66,000)
(2%) $ 92,000 (2%) $(44,000)
(1%) $ 45,000 (1%) $(23,000)
1% $ (43,000) 1% $ 20,000
2% $ (84,000) 2% $ 42,000
3% $(123,000) 3% $ 63,000
(a) Reflects estimated potential changes in medical and other expenses payable caused by changes in
completion factors for incurred months prior to the most recent three months.
42