Humana 2004 Annual Report Download - page 29
Download and view the complete annual report
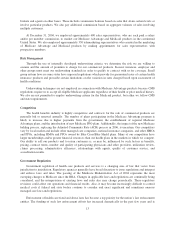
Please find page 29 of the 2004 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.On December 9, 2004, the Court issued an order rescheduling the trial for September 6, 2005. On February
10, 2005, the Court ruled that the trial would be bifurcated so that the issue of liability would be tried first,
followed by proof of damages, if liability is found.
Meanwhile, on September 17, 2004, the plaintiffs filed an amended motion for class certification, seeking a
global fee-for-service class and five subclasses for the time period from January 1, 1996, to the date of
certification. The global class would consist of any medical doctor who provided service on a fee-for-service
basis to any person insured by Cigna Corporation or any other defendant for claims of RICO conspiracy and
aiding and abetting. The motion seeks subclasses for the conspiracy counts for capitation damages and capitation
injunctive relief consisting of all medical doctors who provided services on a capitated basis. The motion also
requests a subclass for a direct RICO claim consisting of medical doctors who provided services on a fee-for-
service basis to any person insured by Humana pursuant to a contract without an arbitration clause or without a
contract. The motion, which has not been ruled on, also seeks two California subclasses, one involving
physicians who provided services on a fee-for-service basis and the other for capitated physicians.
Two of the defendants, Aetna Inc. and Cigna Corporation, have entered into settlement agreements which
have been approved by the Court.
We intend to continue to defend this action vigorously.
Government Audits and Other Litigation and Proceedings
Insurance Industry Brokerage Practices Matters
We have responded to requests for information from the Departments of Insurance in the states of Ohio and
North Carolina with respect to an industry wide investigation into certain insurance brokerage practices,
including broker compensation arrangements, and bid quoting practices. In connection with this industry wide
review, we may receive requests for information or subpoenas from other regulators or attorneys general. We
intend to cooperate fully with any inquiries.
Other
In July 2000, the Office of the Florida Attorney General initiated an investigation, apparently relating to
some of the same matters that are involved in the managed care industry purported class action litigation
described above. On September 21, 2001, the Texas Attorney General initiated a similar investigation. No actions
have been filed against us by either state. These investigations are ongoing, and we have cooperated with the
regulators in both states.
On May 31, 2000, we entered into a five-year Corporate Integrity Agreement, or CIA, with the Office of
Inspector General, or OIG, of the Department of Health and Human Services. Under the CIA, we are obligated
to, among other things, provide training, conduct periodic audits and make periodic reports to the OIG.
In addition, our business practices are subject to review by various state insurance and health care regulatory
authorities and federal regulatory authorities. There has been increased scrutiny by these regulators of the
managed health care companies’ business practices, including allegations of anticompetitive and unfair business
activities, claims payment practices, commission payment practices, and utilization management practices. We
have been and continue to be subject to such reviews. Some of these have resulted in fines and could require
changes in some of our practices and could also result in additional fines or other sanctions.
We also are involved in other lawsuits that arise in the ordinary course of our business operations, including
claims of medical malpractice, bad faith, nonacceptance or termination of providers, improper rate setting, failure
to disclose network discounts and various other provider arrangements, as well as challenges to subrogation
practices. We also are subject to claims relating to performance of contractual obligations to providers, members,
19