Humana 2004 Annual Report Download - page 17
Download and view the complete annual report
Please find page 17 of the 2004 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.In the Balanced Budget Act of 1997 (BBA), Congress created a new rate-setting methodology, eliminating
the direct link in the AAPCC method between managed care rates and local fee-for-service costs. Congress broke
the direct link by requiring that each year a county rate was the highest of three types of rates, each calculated
differently than the old AAPCC rate. As a result, the wide disparities in county capitation rates were reduced by
bringing both high and low payment rates closer to the national average.
Additionally, the BBA required CMS to implement a risk adjustment payment system for Medicare health
plans. Risk adjustment uses health status indicators to improve the accuracy of payments and establish incentives
for plans to enroll and treat less healthy Medicare beneficiaries. CMS initially phased-in this payment
methodology with a risk adjustment model that based payment on principal hospital inpatient diagnoses, as well
as demographic factors such as gender, age, and Medicaid eligibility. From 2000 to 2003, risk adjusted payment
accounted for only 10 percent of Medicare health plans payment, with the remaining 90 percent being based on
demographic factors described above.
Pursuant to the Benefits and Improvements Protection Act of 2000 (BIPA), CMS implemented a new risk
adjustment model that uses additional diagnosis data from ambulatory treatment settings (hospital outpatient
department and physician visits). CMS has also redesigned its data collection and processing system to further
reduce administrative data burden on Medicare health plans. In 2004, the portion of risk adjusted payment was
increased to 30 percent, from 10 percent in 2003. The 100% phase-in of risk adjusted payment will be completed
in 2007; the portion of risk adjusted payment will increase to 50 percent in 2005 and 75 percent in 2006.
Under the new risk adjustment methodology, Humana and all managed care organizations must capture,
collect, and submit the necessary diagnosis code information to CMS twice a year. As a result of this process and
the phasing in of the risk adjustment methodology described above, our CMS monthly payments per member
may change materially, either favorably or unfavorably.
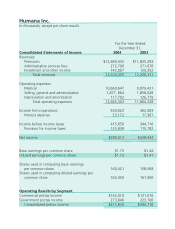
Over the five-year period beginning January 1, 2000 and ending December 31, 2004, our annual increases in
per member premiums from CMS have ranged from as low as approximately 2% to as high as approximately
12%, with an average of approximately 5%. During 2004, we experienced average overall increases in per
member premiums in the range of 9% to 11%. We are expecting a similar level of increase during 2005.
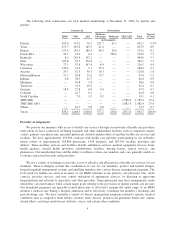
At December 31, 2004, we provided health insurance coverage under CMS contracts to approximately
377,200 Medicare Advantage members for which we received premium revenues of approximately $3.1 billion,
or 23.9% of our total premiums and ASO fees for 2004. One such CMS contract covered approximately 231,700
members in South Florida and accounted for premium revenues of approximately $2.0 billion, which represented
64.9% of our Medicare Advantage premium revenues, or 15.4% of our total premiums and ASO fees for 2004.
Additionally, on February 16, 2005 we acquired CarePlus Health Plans of Florida, adding approximately 50,000
Medicare Advantage HMO members to our South Florida operations.
Our HMO, PPO and PFFS products covered under Medicare Advantage contracts with CMS are renewed
for a one-year term each December 31 unless notice of termination is received at least 90 days prior thereto. No
termination notices were received in connection with our currently existing plans. Additionally, in 2004, we have
established Medicare PFFS plans in eleven states and, have recently established Medicare PPO plans in many of
our existing markets where we have established competitive provider networks. We continue to evaluate
additional states and local markets where we believe we can be competitive with these products, and we
anticipate further expansion during 2005.
Medicaid Product
Medicaid is a federal program that is state-operated to facilitate the delivery of health care services to low-
income residents. Each electing state develops, through a state specific regulatory agency, a Medicaid managed
care initiative that must be approved by CMS. CMS requires that Medicaid managed care plans meet federal
standards and cost no more than the amount that would have been spent on a comparable fee-for-service basis.
States currently either use a formal proposal process in which they review many bidders before selecting one or
award individual contracts to qualified bidders who apply for entry to the program. In either case, the contractual
7