Humana 2004 Annual Report Download - page 18
Download and view the complete annual report
Please find page 18 of the 2004 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.relationship with a state generally is for a one-year period. Under these contracts, we receive a fixed monthly
payment from a government agency for which we are required to provide health insurance coverage to enrolled
members. Due to the increased emphasis on state health care reform and budgetary constraints, more states are
utilizing a managed care product in their Medicaid programs.
We currently have Medicaid contracts with the Puerto Rico Health Insurance Administration through June
30, 2005. Our other Medicaid contracts are in Florida and Illinois, and are annual contracts. For the year ended
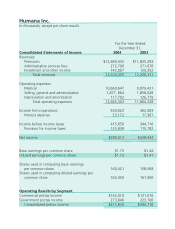
December 31, 2004, premium revenues from our Medicaid products totaled $511.2 million, or 3.9% of our total
premiums and ASO fees. At December 31, 2004, we had approximately 396,600 Medicaid members in Puerto
Rico, or 83% of total Medicaid members, and 82,000 Medicaid members in Florida and Illinois, or 17% of total
Medicaid members.
TRICARE
TRICARE provides health insurance coverage to the dependents of active duty military personnel and to
retired military personnel and their dependents. Currently, three health benefit options are available to TRICARE
beneficiaries. In addition to a traditional indemnity option, participants may enroll in an HMO-like plan with a
point-of-service option or take advantage of reduced copayments by using a network of preferred providers.
We have participated in the TRICARE program since 1996 under contracts with the United States
Department of Defense. Our current TRICARE South Region contract, which we were awarded in 2003, covers
approximately 2.9 million eligible beneficiaries in Florida, Georgia, South Carolina, Mississippi, Alabama,
Tennessee, Louisiana, Arkansas, Texas and Oklahoma. The South Region is one of the three regions in the
United States as defined by the Department of Defense. The TRICARE South Region contract is for a five-year
period subject to annual renewals at the federal government’s option, with the second option period scheduled to
begin April 1, 2005. We have subcontracted with third parties to provide selected administration and specialty
services under the contract.
During 2004, we completed a contractual transition of our TRICARE business. On July 1, 2004, our
Regions 2 and 5 contract servicing approximately 1.1 million TRICARE members became part of the new North
Region, which was awarded to another contractor. On August 1, 2004, our Regions 3 and 4 contract became part
of our new South Region contract. On November 1, 2004, the Region 6 contract, previously administered by the
same contractor, with approximately 1 million members, became part of the South Region contract. The
members added with the Region 6 contract essentially offset the members lost four months earlier with the
Regions 2 and 5 contract. For the year ended December 31, 2004, TRICARE premium revenues were
approximately $2.1 billion, or 16.4% of our total premiums and ASO fees.
At December 31, 2004, we had 1,082,400 TRICARE ASO members representing active duty beneficiaries,
seniors over the age of 65 and beneficiaries in Puerto Rico for which the Department of Defense retains all of the
risk of financing the cost of their health benefit. Part of the TRICARE transition during 2004 included the carve
out of the TRICARE Senior Pharmacy and TRICARE for Life program which we previously administered. On
June 1, 2004 and August 1, 2004, administrative services under these programs were transferred to another
contractor. For the year ended December 31, 2004, TRICARE administrative services fees totaled $106.8
million, or 0.8% of our total premiums and ASO fees.
8