Humana 2011 Annual Report Download - page 24
Download and view the complete annual report
Please find page 24 of the 2011 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.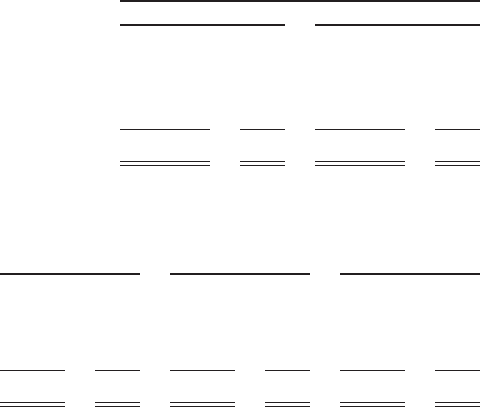
physicians have assumed some level of risk for all or a portion of the medical costs of their HMO membership.
Although these arrangements do include physician capitation payments for services rendered, we share hospital
and other benefit expenses and process substantially all of the claims under these arrangements.
Physicians under capitation arrangements typically have stop loss coverage so that a physician’s financial
risk for any single member is limited to a maximum amount on an annual basis. We monitor the financial
performance and solvency of our capitated providers. However, we remain financially responsible for health care
services to our members in the event our providers fail to provide such services.
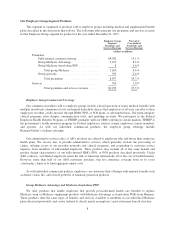
Medical membership under these various arrangements was as follows at December 31, 2011 and 2010:
Medical Membership
December 31, 2011 December 31, 2010
Capitated HMO hospital system based ............. 34,400 0.3% 34,800 0.3%
Capitated HMO physician group based ............ 75,100 0.7% 52,500 0.5%
Risk-sharing ................................. 963,600 8.6% 910,700 8.9%
Other ....................................... 10,111,500 90.4% 9,288,600 90.3%
Total ................................... 11,184,600 100.0% 10,286,600 100.0%
Capitation expense as a percentage of total benefit expense was as follows for the years ended December 31,
2011, 2010, and 2009:
2011 2010 2009
(dollars in millions)
Benefit Expenses:
Capitated HMO expense ............ $ 505 1.8% $ 436 1.6% $ 459 1.9%
Other benefit expense .............. 28,318 98.2% 26,681 98.4% 24,325 98.1%
Consolidated benefit expense ........ $28,823 100.0% $27,117 100.0% $24,784 100.0%
Accreditation Assessment
Our accreditation assessment program consists of several internal programs, including those that credential
providers and those designed to meet the audit standards of federal and state agencies, as well as external
accreditation standards. We also offer quality and outcome measurement and improvement programs such as the
Health Care Effectiveness Data and Information Sets, or HEDIS, which is used by employers, government
purchasers and the National Committee for Quality Assurance, or NCQA, to evaluate health plans based on
various criteria, including effectiveness of care and member satisfaction.
Physicians participating in our networks must satisfy specific criteria, including licensing, patient access,
office standards, after-hours coverage, and other factors. Most participating hospitals also meet accreditation
criteria established by CMS and/or the Joint Commission on Accreditation of Healthcare Organizations.
Recredentialing of participating providers occurs every two to three years, depending on applicable state
laws. Recredentialing of participating physicians includes verification of their medical licenses; review of their
malpractice liability claims histories; review of their board certifications, if applicable; and review of applicable
quality information. A committee, composed of a peer group of physicians, reviews the applications of
physicians being considered for credentialing and recredentialing.
We request accreditation for certain of our health plans and/or departments from NCQA, the Accreditation
Association for Ambulatory Health Care, and the Utilization Review Accreditation Commission, or URAC.
Accreditation or external review by an approved organization is mandatory in the states of Florida and Kansas for
licensure as an HMO. Certain commercial businesses, like those impacted by a third-party labor agreement or
those where a request is made by the employer, may require or prefer accredited health plans.
14