Humana 2011 Annual Report Download - page 72
Download and view the complete annual report
Please find page 72 of the 2011 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.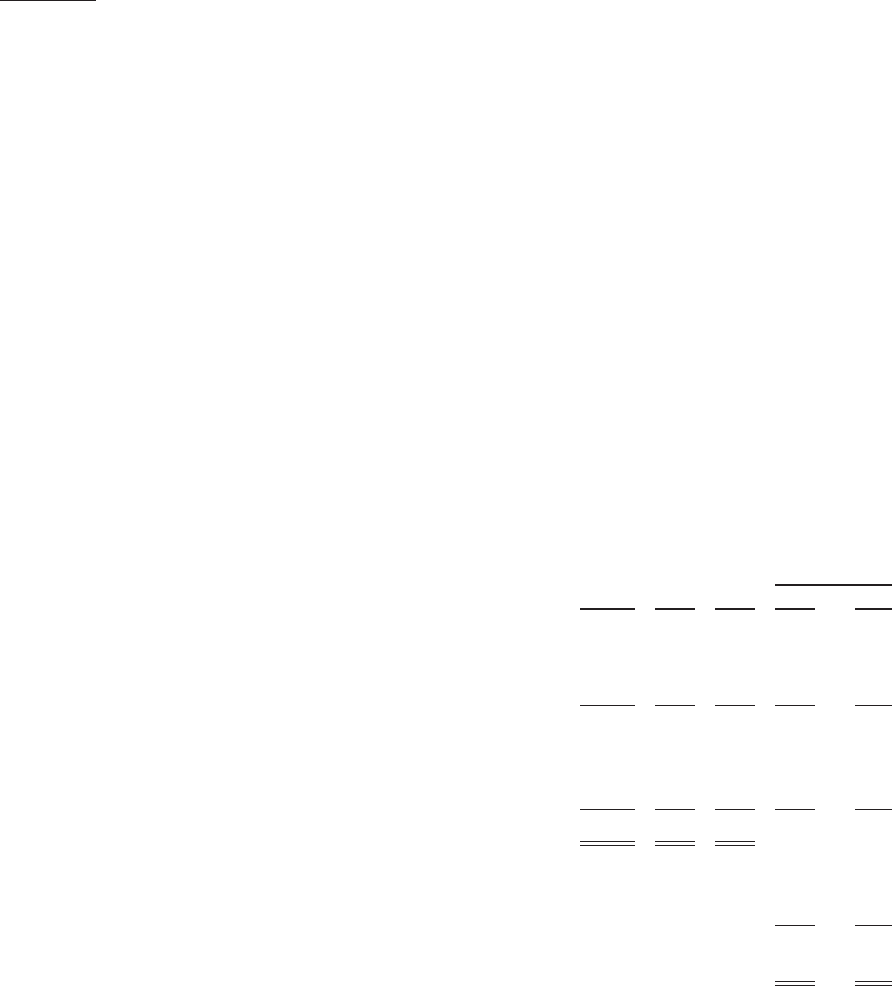
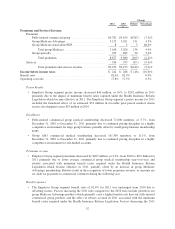
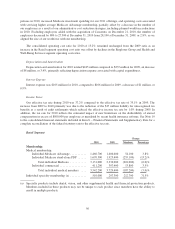
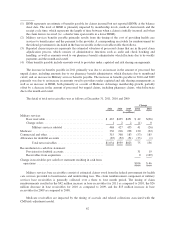
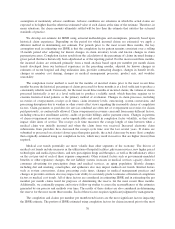
(1) IBNR represents an estimate of benefits payable for claims incurred but not reported (IBNR) at the balance
sheet date. The level of IBNR is primarily impacted by membership levels, medical claim trends and the
receipt cycle time, which represents the length of time between when a claim is initially incurred and when
the claim form is received (i.e. a shorter time span results in a lower IBNR).
(2) Military services benefits payable primarily results from the timing of the cost of providing health care
services to beneficiaries and the payment to the provider. A corresponding receivable for reimbursement by
the federal government is included in the base receivable in the receivables table that follows.
(3) Reported claims in process represents the estimated valuation of processed claims that are in the post claim
adjudication process, which consists of administrative functions such as audit and check batching and
handling, as well as amounts owed to our pharmacy benefit administrator which fluctuate due to bi-weekly
payments and the month-end cutoff.
(4) Other benefits payable include amounts owed to providers under capitated and risk sharing arrangements.
The increase in benefits payable in 2011 primarily was due to an increase in the amount of processed but
unpaid claims, including amounts due to our pharmacy benefit administrator, which fluctuate due to month-end
cutoff, and an increase in Military services benefits payable. The increase in benefits payable in 2010 and 2009
primarily was due to an increase in amounts owed to providers under capitated and risk sharing arrangements as
well as an increase in IBNR, both primarily as a result of Medicare Advantage membership growth, partially
offset by a decrease in the amount of processed but unpaid claims, including pharmacy claims, which fluctuate
due to the month-end cutoff.
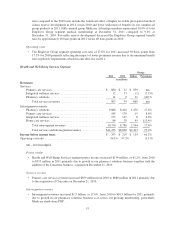
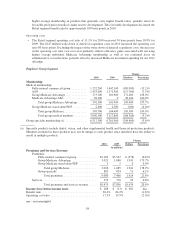
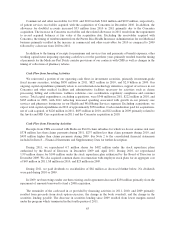
The detail of total net receivables was as follows at December 31, 2011, 2010 and 2009:
Change
2011 2010 2009 2011 2010
(in millions)
Military services:
Base receivable ....................................... $ 467 $425 $451 $ 42 $(26)
Change orders ........................................ 1 2 2 (1) 0
Military services subtotal ........................... 468 427 453 41 (26)
Medicare ................................................ 336 216 238 120 (22)
Commercial and other ...................................... 315 368 183 (53) 185
Allowance for doubtful accounts ............................. (85) (52) (51) (33) (1)
Total net receivables ............................... $1,034 $959 $823 75 136
Reconciliation to cash flow statement:
Provision for doubtful accounts .......................... 31 19
Receivables from acquisition ............................ 0 (109)
Change in receivables per cash flow statement resulting in cash from
operations ............................................. $106 $ 46
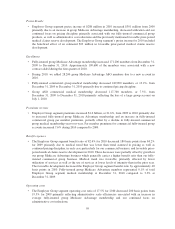
Military services base receivables consist of estimated claims owed from the federal government for health
care services provided to beneficiaries and underwriting fees. The claim reimbursement component of military
services base receivables is generally collected over a three to four month period. The timing of claim
reimbursements resulted in the $42 million increase in base receivables for 2011 as compared to 2010, the $26
million decrease in base receivables for 2010 as compared to 2009, and the $15 million increase in base
receivables for 2009 as compared to 2008.
Medicare receivables are impacted by the timing of accruals and related collections associated with the
CMS risk-adjustment model.
62