Humana 2010 Annual Report Download - page 75
Download and view the complete annual report
Please find page 75 of the 2010 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
The completion factor method is used for the months of incurred claims prior to the most recent three
months because the historical percentage of claims processed for those months is at a level sufficient to produce a
consistently reliable result. Conversely, for the most recent three months of incurred claims, the volume of claims
processed historically is not at a level sufficient to produce a reliable result, which therefore requires us to
examine historical trend patterns as the primary method of evaluation. Changes in claim processes, including
receipt cycle times, claim inventory levels, recoveries of overpayments, outsourcing, system conversions, and
processing disruptions due to weather or other events affect views regarding the reasonable choice of completion
factors. The receipt cycle time measures the average length of time between when a medical claim was initially
incurred and when the claim form was received. Increased electronic claim submissions from providers have
decreased the receipt cycle time over the last few years. For example, the average receipt cycle time has
decreased from 15.0 days in 2008 to 13.8 days in 2010 which represents an 8.0% reduction in cycle time over the
three year period. If claims are submitted or processed on a faster (slower) pace than prior periods, the actual
claim may be more (less) complete than originally estimated using our completion factors, which may result in
reserves that are higher (lower) than required.
Medical cost trends potentially are more volatile than other segments of the economy. The drivers of
medical cost trends include increases in the utilization of hospital facilities, physician services, new higher priced
technologies and medical procedures, and new prescription drugs and therapies, as well as the inflationary effect
on the cost per unit of each of these expense components. Other external factors such as government-mandated
benefits or other regulatory changes, the tort liability system, increases in medical services capacity, direct to
consumer advertising for prescription drugs and medical services, an aging population, lifestyle changes
including diet and smoking, catastrophes, and epidemics also may impact medical cost trends. Internal factors
such as system conversions, claims processing cycle times, changes in medical management practices and
changes in provider contracts also may impact our ability to accurately predict estimates of historical completion
factors or medical cost trends. All of these factors are considered in estimating IBNR and in estimating the per
member per month claims trend for purposes of determining the reserve for the most recent three months.
Additionally, we continually prepare and review follow-up studies to assess the reasonableness of the estimates
generated by our process and methods over time. The results of these studies are also considered in determining
the reserve for the most recent three months. Each of these factors requires significant judgment by management.
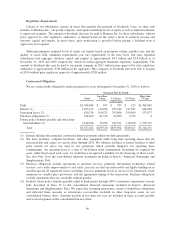
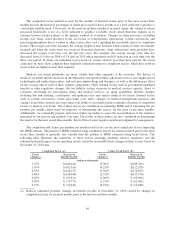
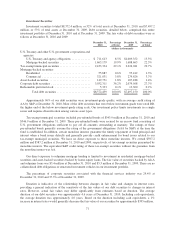
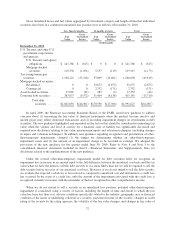
The completion and claims per member per month trend factors are the most significant factors impacting
the IBNR estimate. The portion of IBNR estimated using completion factors for claims incurred prior to the most
recent three months is generally less variable than the portion of IBNR estimated using trend factors. The
following table illustrates the sensitivity of these factors assuming moderate adverse experience and the
estimated potential impact on our operating results caused by reasonably likely changes in these factors based on
December 31, 2010 data:
Completion Factor (a): Claims Trend Factor (b):
Factor
Change (c)
Decrease in
Benefits Payable
Factor
Change (c)
Decrease in
Benefits Payable
(dollars in thousands)
1.25% $(184,444) (5.00)% $(249,764)
1.10% $(162,310) (4.25)% $(212,299)
0.95% $(140,177) (3.50)% $(174,835)
0.80% $(118,044) (2.75)% $(137,370)
0.65% $ (95,911) (2.00)% $ (99,906)
0.50% $ (73,777) (1.25)% $ (62,441)
0.35% $ (51,644) (0.25)% $ (12,488)
(a) Reflects estimated potential changes in benefits payable at December 31, 2010 caused by changes in
completion factors for incurred months prior to the most recent three months.
65