Humana 2013 Annual Report Download - page 110
Download and view the complete annual report
Please find page 110 of the 2013 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Humana Inc.
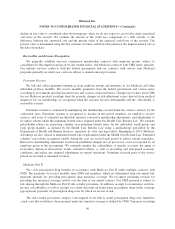
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
referred to as a component, which comprise our reportable segments. A component is considered a reporting unit
if the component constitutes a business for which discrete financial information is available that is regularly
reviewed by management. We aggregate the components of an operating segment into one reporting unit if they
have similar economic characteristics. Goodwill is assigned to the reporting unit that is expected to benefit from
a specific acquisition.
We use a two-step process to review goodwill for impairment. The first step is a screen for potential
impairment, and the second step measures the amount of impairment, if any. Impairment tests are performed, at a
minimum, in the fourth quarter of each year supported by our long-range business plan and annual planning
process. We rely on an evaluation of future discounted cash flows to determine fair value of our reporting units.
Impairment tests completed for 2013, 2012, and 2011 did not result in an impairment loss.
Other intangible assets primarily relate to acquired customer contracts/relationships and are included with
other long-term assets in the consolidated balance sheets. Other intangible assets are amortized over the useful
life, based upon the pattern of future cash flows attributable to the asset. This sometimes results in an accelerated
method of amortization for customer contracts because the asset tends to dissipate at a more rapid rate in earlier
periods. Other than customer contracts, other intangible assets generally are amortized using the straight-line
method. We review other finite-lived intangible assets for impairment under our long-lived asset policy.
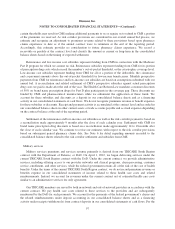
Benefits Payable and Benefits Expense Recognition
Benefits expense includes claim payments, capitation payments, pharmacy costs net of rebates, allocations
of certain centralized expenses and various other costs incurred to provide health insurance coverage to members,
as well as estimates of future payments to hospitals and others for medical care and other supplemental benefits
provided prior to the balance sheet date. Capitation payments represent monthly contractual fees disbursed to
primary care and other providers who are responsible for providing medical care to members. Pharmacy costs
represent payments for members’ prescription drug benefits, net of rebates from drug manufacturers. Receivables
for such pharmacy rebates are included in other current assets in the consolidated balance sheets. Other
supplemental benefits include dental, vision, and other supplemental health and financial protection products.
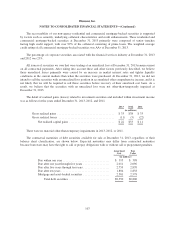
We estimate the costs of our benefits expense payments using actuarial methods and assumptions based
upon claim payment patterns, medical cost inflation, historical developments such as claim inventory levels and
claim receipt patterns, and other relevant factors, and record benefit reserves for future payments. We continually
review estimates of future payments relating to claims costs for services incurred in the current and prior periods
and make necessary adjustments to our reserves.
We reassess the profitability of our contracts for providing insurance coverage to our members when current
operating results or forecasts indicate probable future losses. We establish a premium deficiency liability in
current operations to the extent that the sum of expected future costs, claim adjustment expenses, and
maintenance costs exceeds related future premiums under contracts without consideration of investment income.
For purposes of determining premium deficiencies, contracts are grouped in a manner consistent with our method
of acquiring, servicing, and measuring the profitability of such contracts. Losses recognized as a premium
deficiency result in a beneficial effect in subsequent periods as operating losses under these contracts are charged
to the liability previously established. Because the majority of our member contracts renew annually, we do not
anticipate recording a material premium deficiency liability, except when unanticipated adverse events or
changes in circumstances indicate otherwise.
We believe our benefits payable are adequate to cover future claims payments required. However, such
estimates are based on knowledge of current events and anticipated future events. Therefore, the actual liability
could differ materially from the amounts provided.
100