Humana 2013 Annual Report Download - page 57
Download and view the complete annual report
Please find page 57 of the 2013 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.• Automatic across-the-board budget cuts under the Budget Control Act of 2011 and the American
Taxpayer Relief Act of 2012, known as “sequestration,” commenced in March 2013, including a 2%
reduction in Medicare Advantage and Medicare Part D payments beginning April 1, 2013. While we
believe we can reduce Medicare Advantage payments to providers under our network provider
contracts in connection with sequestration, a number of hospitals and other providers have asserted that
we are not entitled to do so, which have led and may lead to arbitration demands or other litigation
regarding these matters. While we believe our senior members’ benefits may be adversely impacted,
we believe we can effectively design Medicare Advantage products based upon these levels of rate
reduction while continuing to remain competitive compared to both the combination of original
Medicare with a supplement policy as well as Medicare Advantage products offered by our
competitors. Nonetheless, there can be no assurance that we will be able to successfully execute
operational and strategic initiatives that we have assumed when designing our plan benefit offerings
and premiums for 2014. Failure to execute these strategies may result in a material adverse effect on
our results of operations, financial position, and cash flows.
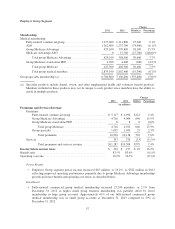
• For the year ended December 31, 2013, our Retail segment pretax income grew by 10.5%, primarily
driven by individual Medicare Advantage and Medicare stand-alone PDP membership growth in
excess of 7%.
• January 2014 individual Medicare Advantage membership increased approximately 250,000 members,
or 12%, from December 31, 2013. January 2014 Medicare stand-alone PDP membership, excluding the
LI-NET prescription drug plan program, increased approximately 500,000 members, or 16%, from
December 31, 2013. These increases reflect net membership additions for the 2014 enrollment season.
• Star Ratings issued by CMS in October 2013 indicated that 55% to 60% of our Medicare Advantage
members are now in plans with an overall Star Rating of four or more stars. We have 18 Medicare
Advantage plans that achieved a rating of four or more stars, an increase of 50% from the previous
year. We are offering nine Medicare Advantage plans that achieved a 4.5 Star Rating. Beginning in
2015, plans must have a Star Rating of four or higher to qualify for quality bonuses in the basic
premium rates.
• We were successful in our bids for state-based contracts in Florida and Virginia in 2013 and Ohio,
Illinois, and Kentucky in 2012. Ohio, Illinois, and Virginia are contracts for stand-alone dual eligible
demonstration programs serving individuals dually eligible for both the federal Medicare program and
the state-based Medicaid program. We partner with organizations, including CareSource Management
Group Company, to serve individuals in certain states. Medicaid membership in our Retail Segment at
December 31, 2013 increased 33,400 members from December 31, 2012, primarily driven by the
addition of our Kentucky Medicaid contract effective January 1, 2013 and Florida Long-Term Support
Services contracts in certain regions, including American Eldercare Inc. We expect to begin serving
new members in Ohio, Illinois, Virginia, and Florida at various dates between the first quarter and third
quarter of 2014. While we expect the Medicaid and dual-eligible demonstration business to result in
future growth, the mix of lower margin Medicaid and dual-eligible demonstration business with the
higher margin Medicare Advantage business may result in a decline in Retail segment margins over
time.
• On September 6, 2013, we acquired American Eldercare Inc., or American Eldercare, the largest
provider of nursing home diversion services in the state of Florida, serving frail and elderly individuals
in home and community-based settings. American Eldercare complements our core capabilities and
strength in serving seniors and disabled individuals with a unique focus on individualized and
integrated care, and has contracts to provide Medicaid long-term support services across the entire state
of Florida. The enrollment effective dates for the various regions range from August 2013 to March
2014.
• While we do not expect our quarterly earnings progression to be significantly different from our
recurring historical patterns, we do anticipate a slightly lower earnings run rate in the first half of 2014
due to the continuing administrative spending to support our state-based contracts.
47