Humana 2013 Annual Report Download - page 91
Download and view the complete annual report
Please find page 91 of the 2013 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Premiums revenue and administrative services only, or ASO, fees are estimated by multiplying the
membership covered under the various contracts by the contractual rates. In addition, we adjust revenues for
estimated changes in an employer’s enrollment and individuals that ultimately may fail to pay, and for estimated
rebates under the minimum benefit ratios required under the Health Care Reform Law. We estimate policyholder
rebates by projecting calendar year minimum benefit ratios for the individual, small group, and large group
markets, as defined by the Health Care Reform Law using a methodology prescribed by the Department of
Health and Human Services, separately by state and legal entity. Beginning in 2014, Medicare Advantage plans
are also subject to minimum benefit ratio requirements under the Health Care Reform Law. Estimated calendar
year rebates recognized ratably during the year are revised each period to reflect current experience. Enrollment
changes not yet processed or not yet reported by an employer group or the government, also known as retroactive
membership adjustments, are estimated based on available data and historical trends. We routinely monitor the
collectibility of specific accounts, the aging of receivables, historical retroactivity trends, estimated rebates, as
well as prevailing and anticipated economic conditions, and reflect any required adjustments in the current
period’s revenue.
We bill and collect premium remittances from employer groups and members in our Medicare and other
individual products monthly. We receive monthly premiums from the federal government and various states
according to government specified payment rates and various contractual terms. Changes in revenues from CMS
for our Medicare products resulting from the periodic changes in risk-adjustment scores derived from medical
diagnoses for our membership are recognized when the amounts become determinable and the collectibility is
reasonably assured.
Medicare Part D Provisions
We cover prescription drug benefits in accordance with Medicare Part D under multiple contracts with
CMS. The payments we receive monthly from CMS and members, which are determined from our annual bid,
represent amounts for providing prescription drug insurance coverage. We recognize premiums revenue for
providing this insurance coverage ratably over the term of our annual contract. Our CMS payment is subject to
risk sharing through the Medicare Part D risk corridor provisions. In addition, receipts for reinsurance and low-
income cost subsidies as well as receipts for certain discounts on brand name prescription drugs in the coverage
gap represent payments for prescription drug costs for which we are not at risk.
The risk corridor provisions compare costs targeted in our bids to actual prescription drug costs, limited to
actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding
certain thresholds may result in CMS making additional payments to us or require us to refund to CMS a portion
of the premiums we received. As risk corridor provisions are considered in determining the rate, we estimate and
recognize an adjustment to premiums revenue related to these risk corridor provisions based upon pharmacy
claims experience to date as if the annual contract were to terminate at the end of the reporting period.
Accordingly, this estimate provides no consideration to future pharmacy claims experience. We record a
receivable or payable at the contract level and classify the amount as current or long-term in the consolidated
balance sheets based on the timing of expected settlement.
The estimate of the settlement associated with risk corridor provisions requires us to consider factors that
may not be certain at period end, including member eligibility and risk adjustment score differences with CMS as
well as pharmacy rebates from manufacturers. These factors have an offsetting effect on changes in the risk
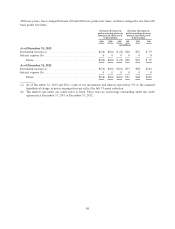
corridor estimate. In 2013, we paid $207 million related to our reconciliation with CMS regarding the 2012
Medicare Part D risk corridor provisions compared to our estimate of $194 million at December 31, 2012. In
2012, we paid $131 million and in January 2013 we paid $158 million related to our reconciliation with CMS
regarding the 2011 Medicare Part D risk corridor provisions compared to our estimate of $286 million at
December 31, 2011. In 2011, we paid $380 million related to our reconciliation with CMS regarding the 2010
Medicare Part D risk corridor provisions compared to our estimate of $345 million at December 31, 2010. The
net liability associated with the 2013 risk corridor estimate, which will be settled in 2014, was $46 million at
December 31, 2013.
81