Humana 2013 Annual Report Download - page 92
Download and view the complete annual report
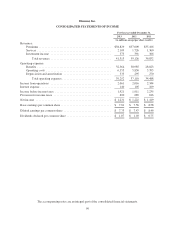
Please find page 92 of the 2013 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Reinsurance and low-income cost subsidies represent funding from CMS in connection with the Medicare
Part D program for which we assume no risk. Reinsurance subsidies represent funding from CMS for its portion
of prescription drug costs which exceed the member’s out-of-pocket threshold, or the catastrophic coverage level.
Low-income cost subsidies represent funding from CMS for all or a portion of the deductible, the coinsurance
and co-payment amounts above the out-of-pocket threshold for low-income beneficiaries. Monthly prospective
payments from CMS for reinsurance and low-income cost subsidies are based on assumptions submitted with our
annual bid. A reconciliation and related settlement of CMS’s prospective subsidies against actual prescription
drug costs we paid is made after the end of the year. The Health Care Reform Law mandates consumer discounts
of 50% on brand name prescription drugs for Part D plan participants in the coverage gap. These discounts are
funded by CMS and pharmaceutical manufacturers while we administer the application of these funds. We
account for these subsidies and discounts as a deposit in our consolidated balance sheets and as a financing
activity in our consolidated statements of cash flows. We do not recognize premiums revenue or benefits expense
for these subsidies or discounts. Receipt and payment activity is accumulated at the contract level and recorded in
our consolidated balance sheets in other current assets or trade accounts payable and accrued expenses depending
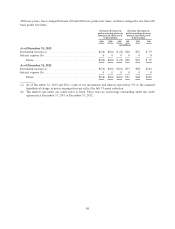
on the contract balance at the end of the reporting period. Gross financing receipts were $4.6 billion and gross
financing withdrawals were $4.8 billion during 2013. CMS subsidy and brand name prescription drug discount
activity recorded to the consolidated balance sheets at December 31, 2013 was $743 million to other current
assets and $30 million to trade accounts payable and accrued expenses.
Settlement of the reinsurance and low-income cost subsidies as well as the risk corridor payment is based on
a reconciliation made approximately 9 months after the close of each calendar year. Settlement with CMS for
brand name prescription drug discounts is based on a reconciliation made approximately 14 to 18 months after
the close of each calendar year. We continue to revise our estimates with respect to the risk corridor provisions
based on subsequent period pharmacy claims data.
Medicare Risk-Adjustment Provisions
CMS utilizes a risk-adjustment model which apportions premiums paid to Medicare Advantage plans
according to health severity. The risk-adjustment model pays more for enrollees with predictably higher costs.
Under the risk-adjustment methodology, all Medicare Advantage plans must collect and submit the necessary
diagnosis code information from hospital inpatient, hospital outpatient, and physician providers to CMS within
prescribed deadlines. The CMS risk-adjustment model uses this diagnosis data to calculate the risk-adjusted
premium payment to Medicare Advantage plans. Rates paid to Medicare Advantage plans are established under
an actuarial bid model, including a process that bases our payments on a comparison of our beneficiaries’ risk
scores, derived from medical diagnoses, to those enrolled in the government’s original Medicare program. We
generally rely on providers, including certain providers in our network who are our employees, to code their
claim submissions with appropriate diagnoses, which we send to CMS as the basis for our payment received
from CMS under the actuarial risk-adjustment model. We also rely on providers to appropriately document all
medical data, including the diagnosis data submitted with claims. We estimate risk-adjustment revenues based on
medical diagnoses for our membership. The risk-adjustment model is more fully described in Item 1. – Business
under the section titled “Individual Medicare.”
Military services
In 2013, revenues associated with our military services business represented approximately 1% of total
premiums and services revenue. Military services premiums and services revenue primarily is derived from our
TRICARE South Region contract with the Department of Defense, or DoD. On April 1, 2012, we began
delivering services under our current TRICARE South Region contract with the DoD. Under the current contract,
we provide administrative services, including offering access to our provider networks and clinical programs,
claim processing, customer service, enrollment, and other services, while the federal government retains all of
the risk of the cost of health benefits. Under the terms of the current TRICARE South Region contract, we do not
record premiums revenue or benefits expense in our consolidated statements of income related to these health
82