Humana 2014 Annual Report Download - page 98
Download and view the complete annual report
Please find page 98 of the 2014 Humana annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Humana Inc.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
90
gross basis. We shared the risk with the federal government for the cost of health benefits incurred under our previous
contract, earning more revenue or incurring additional cost based on the variance of actual health care costs from an
annually negotiated target health care cost. TRICARE revenues under the previous contract consisted generally of
(1) an insurance premium for assuming underwriting risk for the cost of civilian health care services delivered to eligible
beneficiaries; (2) health care services provided to beneficiaries which were in turn reimbursed by the federal government;
and (3) administrative services fees related to claim processing, customer service, enrollment, and other services. We
recognized the insurance premium as revenue ratably over the period coverage was provided. Health care services
reimbursements were recognized as revenue in the period health services were provided. Administrative services fees
were recognized as revenue in the period services were performed. We deferred the recognition of any contingent
revenues for favorable variances until the end of the contract period when the amount was determinable and the
collectibility was reasonably assured. We estimated and recognized contingent benefits expense for unfavorable
variances currently in our results of operations.
Services Revenue
Patient services revenue
Patient services include injury and illness care and related services as well as other healthcare services related to
employer needs or as required by law. Patient services revenues are recognized in the period services are provided to
the customer when the sales price is fixed or determinable, and are net of contractual allowances.
Administrative services fees
Administrative services fees cover the processing of claims, offering access to our provider networks and clinical
programs, and responding to customer service inquiries from members of self-funded groups. Revenues from providing
administration services, also known as administrative services only, or ASO, are recognized in the period services are
performed and are net of estimated uncollectible amounts. ASO fees are estimated by multiplying the membership
covered under the various contracts by the contractual rates. Under ASO contracts, self-funded employers retain the
risk of financing substantially all of the cost of health benefits. However, many ASO customers purchase stop loss
insurance coverage from us to cover catastrophic claims or to limit aggregate annual costs. Accordingly, we have
recorded premiums revenue and benefits expense related to these stop loss insurance contracts. We routinely monitor
the collectibility of specific accounts, the aging of receivables, as well as prevailing and anticipated economic conditions,
and reflect any required adjustments in current operations. ASO fees received prior to the service period are recorded
as unearned revenues.
On April 1, 2012, we began delivering services under our current TRICARE South Region contract with the DoD.
Under the current contract, we provide administrative services, including offering access to our provider networks and
clinical programs, claim processing, customer service, enrollment, and other services, while the federal government
retains all of the risk of the cost of health benefits. We account for revenues under the current contract net of estimated
health care costs similar to an administrative services fee only agreement. The current contract includes fixed
administrative services fees and incentive fees and penalties. Administrative services fees are recognized as services
are performed.
Our TRICARE members are served by both in-network and out-of-network providers in accordance with the
current contract. We pay health care costs related to these services to the providers and are subsequently reimbursed
by the DoD for such payments. We account for the payments of the federal government’s claims and the related
reimbursements under deposit accounting in our consolidated balance sheets and as a financing activity under receipts
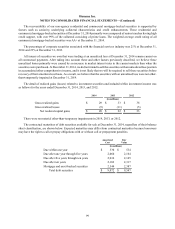
(withdrawals) from contract deposits in our consolidated statements of cash flows. For 2014, health care cost
reimbursements and payments were each approximately $3.2 billion for the year. For 2013, health care cost
reimbursements were $3.2 billion, exceeding payments of $3.2 billion by $5 million. For the first nine months of the
current contract, April 1, 2012 to December 31, 2012, health care cost payments were $2.1 billion, exceeding
reimbursements of $2.0 billion by $56 million.